What is Retinal Vein Occlusion?
As it is the case with any other organ in our body, there are blood vessels that nourish the retina and blood vessels that take the blood rich in carbon dioxide and other waste products from the retina. Blood rich in oxygen and other nutrients enters the retina through the central retinal artery. Deoxygenated blood, on the other hand, leaves the organ via the central retinal vein, once it has been collected from smaller blood vessels and capillaries.
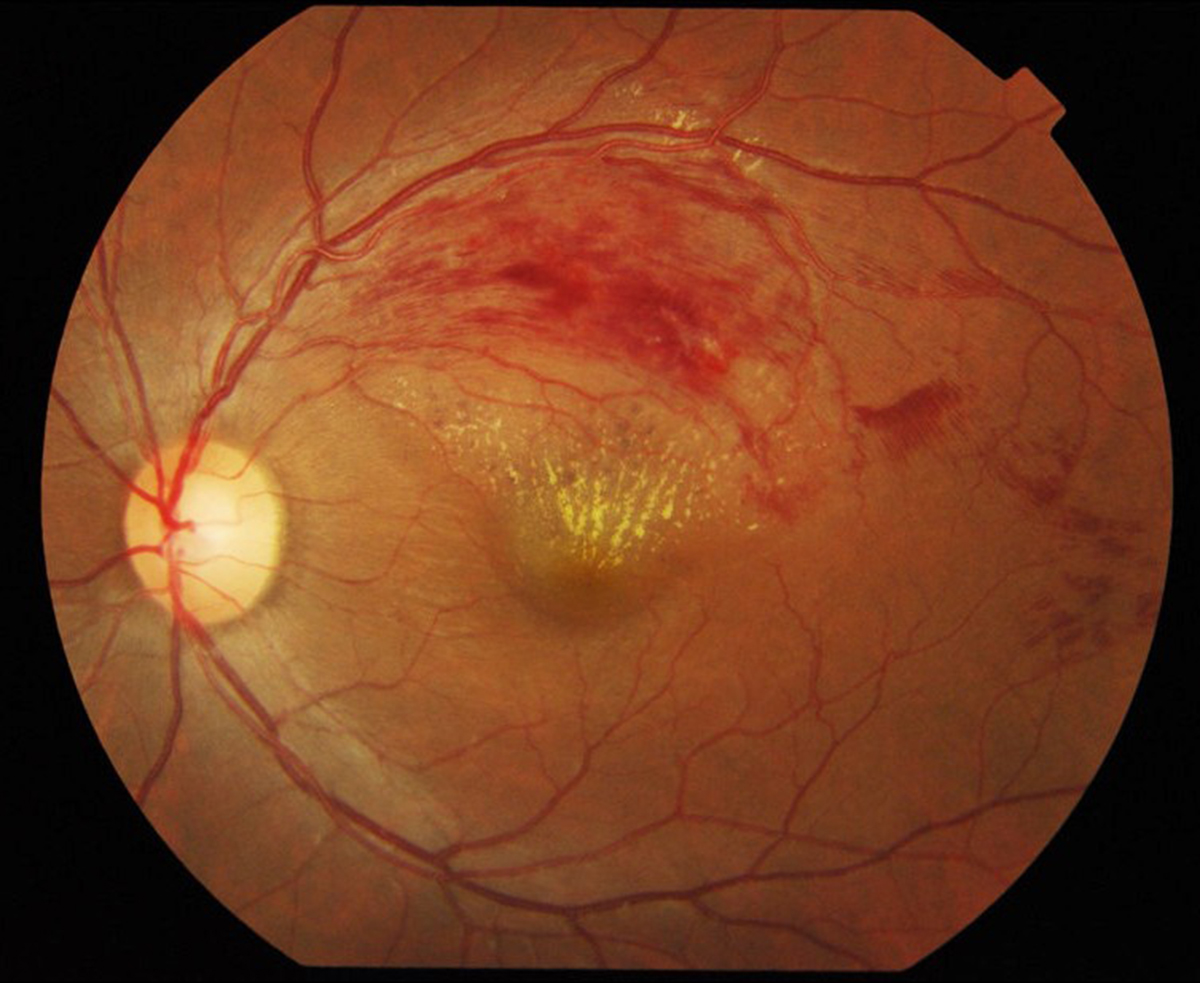
When the central retinal vein gets blocked the person is said to suffer from central retinal vein occlusion. The severity of the condition determines the intensity of symptoms and vision loss. Central retinal vein occlusion is classified into ischemic and non-ischemic.
The condition is equally reported among men and women while it mostly occurs after the age of 50. The disease reaches its peak incidence in individuals in their 60s and 70s. The risk factors for central retinal vein occlusion are practically the same as those associated with stroke and coronary artery disease. Glaucoma, inflammatory or infectious conditions such as sarcoidosis, tuberculosis etc. are also considered potential contributors to the disease.
One of the most common complications of the condition is neovascularization affecting the front of the eye, to be more precise the iris. It subsequently leads to an increase in intraocular pressure, a type of glaucoma known as neovascular glaucoma. The effects of neovascular glaucoma are highly detrimental. Namely, such patients are at great risk of permanent vision loss. Neovascularization may additionally affect the back of the eye, precipitating bleeding into the vitreous and accompanying retinal detachment. Neovascularization, in general, is considered a rather serious complication of the disease. It occurs 6-12 months after the occlusion and if left untreated in approximately 60% leads to bleeding into the vitreous. Finally, certain numbers of patients are confirmed with macular edema, another complication of central retinal vein occlusion.
Although laser therapy, the cornerstone of treatment for central retinal vein occlusion associated neovascularization, might be very successful with practically all complications, it is simple ineffective when the retina gets affected by scar tissues, a complication known under the name a macular pucker or an epiretinal membrane.
How is Central Retinal Vein Occlusion Managed?
In spite of all efforts, the prognosis of central retinal vein occlusion is not so good. All risk factors as well as illnesses which tend to stimulate progression of damage or trigger recurrence of occlusion are supposed to be identified and properly dealt with.
The condition is closely connected with glaucoma, systemic hypertension, tobacco use as well as hyperlipidemia or hypercholesterolemia. Also, it may easily result from atherosclerosis and is reported to affect more people suffering from diabetes and coagulopathies. Therefore, these conditions should be properly managed and central retinal vein occlusion can be prevented. Even if the problem occurs its recurrence may be successfully avoided with more aggressive treatment of the underlying cause. Scientists have confirmed that women taking oral contraceptives are prone to coagulopathies and blood clot formation. This also explains why oral contraceptives are another reason behind central retinal vein occlusion.
One of the efficient drugs that can prevent occlusion not only in the retina but also in other organs in the body is Aspirin. It is supposed to be taken in small doses on a daily basis. Aspirin must never be prescribed to people allergic to the drug no matter how efficient it can be against vascular occlusion.
One of several complications of the condition, macular edema, is treated with intravenously administered bevacuzimab. The drug inhibits proliferation of endothelial cells, vasculogenesis and angiogenesis i.e. blocks the effects of VEGF (vascular endothelial growth factor). Additional help is achieved by corticosteroids. They are also administered intravenously. Since patients with macular edema might need prolonged treatment with steroids which should be maintain within optimal range they are generally recommended sustained-release steroid implants. This is a drug delivery system implanted in the eye that gradually releases corticosteroid to the posterior eye segment.
In more complex cases of the disease, the retina gets affected by neovascularization. New blood vessels start to form which might cause detrimental effects on the vision and trigger additional heath issues. The most severe associated problems are glaucoma and retinal detachment. These complications develop within 6 months after the very occlusion. During this period of time patients are due to have regular eye check-ups. If neovascularization is confirmed, laser therapy is indicated.
Laser photocoagulation therapy is sometimes combined with anti-VEGF therapy. However, conservative approach might not be sufficient enough to prevent new blood vessels from forming or simply cannot deal with subsequent complications. This is when surgery takes place. Vitrectomy is one of the standard procedures done in people suffering from bleeding into the vitreous and threatening retinal detachment. Surgery is also indicated in patients suffering from neovascular glaucoma.
And finally, there is a new treatment tested. It includes injection of anti-vasogenic drugs. The drugs prevent new blood vessels from developing. The results are promising but this treatment approach is yet to be approved.
















Your thoughts on this
Loading...