Partial seizures are also well-known under two other names, focal seizures, and localized seizures. They affect only one part of the brain or one brain hemisphere. Partial seizures can be simple partial seizures and complex partial seizures, which can even lead to extreme cases of generalized seizures.
People who suffer from epilepsy most frequently face this type of seizure. If a simple partial seizure leads to a complex partial seizure then the simple partial seizure is called an aura, and the complex partial seizure is called tonic-clonic seizure.
When it comes to a simple partial seizure, the person stays conscious, but movements, emotions, and sensations are affected. He or she has sudden feelings of fear, anxiety, happiness, nausea, or even a sense of déjà vu may suddenly appear, as well as illusions and hallucinations. The person remembers all when the seizure stops.

Complex partial seizure is commonly known as psychomotor epilepsy. When this kind of seizure happens, the person loses consciousness and becomes unaware, as a sleepwalker. The person stays active performing some actions, for example, undressing, and wanders around, but is unable to interact with other people and has amnesia or cannot remember what was happening during the seizure when she or he returns to the normal state.
Partial Seizures Treatment
Partial seizures must be treated because they can be life-threatening in some cases, or can leave serious damage and impact on the functioning of many organs.
The usual treatment involves medication, surgery, or electrical brain stimulation. Medications can only prevent or control possible seizures in people who suffer from epilepsy but cannot cure epilepsy. The medications must be used every day exactly the way that the physician prescribed them, and without exception. Of all the medications, many anti-epilepsy drugs and anticonvulsants are used for treating partial seizures, but there is no specific one that is the most effective. Anticonvulsants can prevent the return of the seizure. The most common anticonvulsants are Crabamazepine, Divalproex sodium, Gabapentin, Lamotrigine, Phenobarbital, Phenytoin,Fosphentyoin, Primidone, Fiagabine, Topiramate, and Oxcarbazepine.
- This double-blind study was conducted to evaluate the efficacy and safety of gabapentin 1200 mg/day and 1800 mg/day (t.i.d.) compared to placebo as an adjunctive therapy in patients with refractory epilepsy.
- Patients were included when they had partial seizures at least eight times during a 12-week baseline period despite treatment with one to two antiepileptic drugs. After baseline, eligible patients were randomized to gabapentin 1200 mg/day, 1800 mg/day, or placebo for 12-week treatment.
- The primary end-point, response ratio, was derived from seizure frequencies during treatment and baseline period based upon the seizure daily record by a patient.
- Of the 209 randomized patients, 86 received gabapentin 1200 mg/day, 41 received gabapentin 1800 mg/day, and 82 received placebo. A statistically significant difference was found between each of the two gabapentin groups and placebo for the primary efficacy end-point, response ratio (P
- More gabapentin patients reported moderate to marked improvement in seizure frequency and intensity/duration of each seizure than placebo patients. Treatment-related adverse events were reported by approximately 65% of patients receiving gabapentin compared to approximately 46% of patients receiving placebo; somnolence and dizziness were the most common events. Gabapentin 1200 mg/day and 1800 mg/day significantly reduced the frequency of refractory seizures compared to placebo.
If the medications are not much helpful then the surgery is recommended. It includes the removal of the region of the brain where these seizures happen. If the removal cannot be done, then in that case disconnection of the nerve cells is being done. This kind of operation is done to prevent drop attacks, and it is called corpus colostomy.
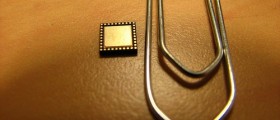
If for some reason, the surgery cannot be performed, then Vagus nerve stimulation (VNS) is suggested. The Vagus nerve is in the neck. For VNS treatment, a small battery must be placed in the chest wall to electrically stimulate the brain with a little burst of energy.
- medlineplus.gov/ency/article/000697.htm
- www.cdc.gov/epilepsy/about/faq.htm
- Photo courtesy of DMTrott by Wikimedia Commons: commons.wikimedia.org/wiki/File:Etizolam.jpg













Your thoughts on this
Loading...