Transient Ischemic Attack (TIA) Overview
Stroke is one of the most debilitating medical conditions. Fortunately, sometime patients who are at risk of stroke first develop transient ischemic attack, an introduction to a stroke and may be timely warned about all the potential complications they might experience unless the underlying conditions or factors contributing to the stroke are not brought under control.
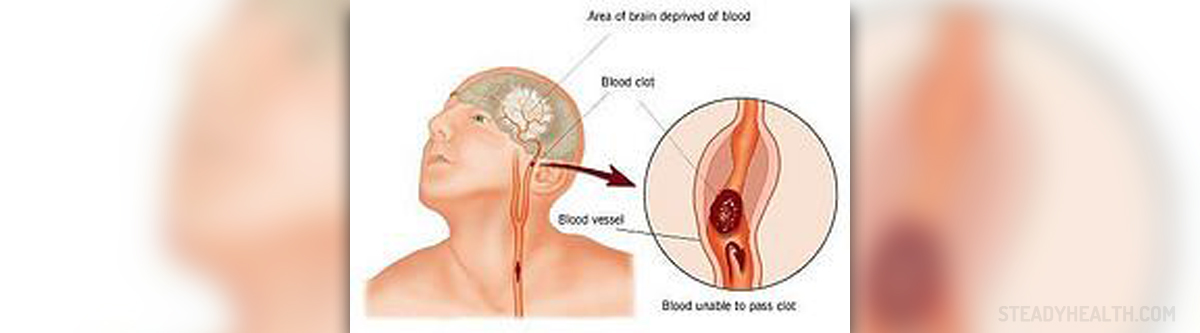
TIA (transient ischemic attack) develops once the blood clot from some part of the body (usually the carotid arteries in the neck) enters the brain arteries and triggers temporary blockage. The obstruction of the affected blood vessel is blamed for blood and oxygen deprivation which precipitates certain changes of brain functions.
Fortunately, the blood flow is soon restored and brain cells suffer no permanent damage. TIA is often referred to as mini-stroke. Unlike the actual stroke there is no irreversible damage to the brain and all the changes in brain function soon get back to normal. The condition can be perceived as a major warning sign of damage that might be permanent unless the person starts with appropriate treatment in order to prevent recurrent cerebrovascular accidents.
The symptoms of transitory ischemic attack usually resolve within 24 hours after the onset although the affected functions are mostly restored within minutes.
Transient Ischemic Attack Symptoms
The symptoms are not unique but depend on the affected portion of the brain i.e. the part of the organ deprived of blood.
Neurological deficits develop rapidly and basically develop on one side of the body, the one opposite the affected side of the brain. Most patients complain about speech and visual problems. They may also appear confused, experience difficulty saying words or be practically unable to understand what people around them are saying.
The symptoms are usually limited to only an arm, leg or a part of the face. Instead of actual paralysis, which is a characteristic of a stroke, patients suffering from TIA usually report numbness, burning sensation or tingling in the affected area. They may additionally experience clumsiness when trying to hold some objects.
In case the blood deprivation takes place in the cerebellum there are dizziness, loss of balance and coordination as well as difficulty walking.
Furthermore, lack of blood supply to the base of the brain results in drop attacks while sudden loss of vision medically known as amaurosis fugax develops as a consequence of the occlusion of the ophthalmic artery.
All in all, any person who develops some of the mentioned is due to call 911 without hesitation. TIA is like a stroke a medical emergency and although patients do recover the initial attack might progress into an actual stroke. The condition is highly unpredictable and requires prompt evaluation and proper treatment. Once administered into a hospital patients undergo series of test and exams, are evaluated for the risks of future stroke and prescribed the most suitable treatment.
Transient Ischemic Attack (TIA) Treatment
The goal of the treatment is to prevent future stroke. There are simple scoring systems available which almost precisely estimate the risk of stroke and determine if there is a necessity for patients to remain hospitalized in order to be further tested. Some patients may be discharged and come to scheduled appointments for further assessment.
Initially, doctors do their best to teach patients how to minimize risk factors. Those with underlying hypertension, increased levels of cholesterol and triglycerides as well as patients suffering from diabetes are due to stick to the prescribed drugs achieving the optimal range of blood pressure, level of lipids in the blood and blood sugar levels.
Most patients are additionally prescribed Aspirin. Low doses of the drug taken on a daily basis prevent platelets from sticking, this way negatively influencing blood clot formation.
Those in whom the carotid arteries are severely narrowed are referred to a vascular surgeon who might recommend carotid endarterectomy.
Unless all the precautionary measures are applied, the risk of stroke within the following months significantly increases. As a matter of fact it is estimated that 10% of patients with TIA develop stroke within 3 months after the initial cerebrovascular incident.
When it comes to prevention of both transient ischemic attack and stroke some risk factors simply cannot be evaded. For instance, we cannot change our genetics or the fact that some family members of ours have had a stoke which are both huge risk factors of the disease. On the other hand, we may prevent or at least postpone hypertension, sometimes diabetes and definitely high level of cholesterol in blood. Smoking is an unhealthy habit and another risk factor that must be eradicated at once.
The prognosis of TIA is good given the complete improvement of neurological deficits. However, surviving the TIA does not mean that one will successfully prevent the potentially forthcoming stroke and all the health problems it brings along. Therefore, take TIA seriously, stick to all the recommendations of the doctor and eliminate all the risk factors which might contribute to stroke.




-Disease-Cause-A-Stroke_f_280x120.jpg)








Your thoughts on this
Loading...