Ventriculoperitoneal Shunt - Overview
Ventriculoperitoneal shunt is a connection between the brain (to be more precise its ventricles) and the peritoneal cavity. This connection is artificial and is necessary for proper drainage of the excess cerebrospinal fluid, which, if not eliminated, causes hydrocephalus. This is the most commonly used path of drainage. In rare cases, cerebrospinal fluid is drained into the chest.
This surgical procedure is performed under general anesthesia and lasts approximately an hour and a half. The surgeon reaches the brain via an incision made behind the patient's ear. The surgeon also makes a small incision in the patient's belly. What follows is the insertion of a catheter into the brain, and another catheter is then tunneled under the skin from behind the ear, down the neck and chest, and finally, it is placed through the incision into the abdominal cavity.
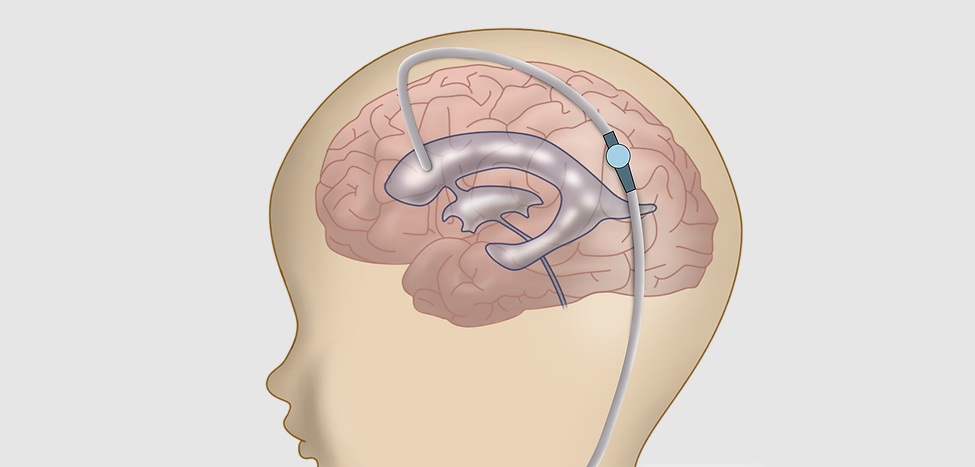
A valve is an essential part of the equipment, and it is inserted under the skin behind the ear. This valve is connected to both catheters. Once the intracranial pressure rises, the excess cerebrospinal fluid is drained from the brain into the abdomen.
Potential Complications of Ventriculoperitoneal Shunt
There are numerous complications related to ventriculoperitoneal shunt. Some of them require prompt revision of the shunt. The most serious of all is shunt failure.
One of the possible complications of ventriculoperitoneal shunt is infection. It affects pediatric patients the most since their immune system is not fully developed. The most common infective agents which lead to infection in patients with a ventriculoperitoneal shunt are Staphylococcus epidermidis, Staphylococcus aureus, and Candida albicans.
Another possible complication is obstruction of the shunt. The shunt may be blocked at the proximal or distal end. The cause of the proximal blockage is an accumulation of excess protein in the cerebrospinal fluid while blockage at the distal end usually occurs due to the pulling of the shunt out of the abdominal cavity.
In some cases the shunt may drain too much cerebrospinal fluid, or the drainage may be way too fast. Both of these complications can lead to serious damage to the brain.
- A retrospective chart review was performed over all shunt implantations from January 2011 to December 2016 within the Houston Methodist Hospital system. Complication rates within 6 months of the operative date, including infection, subdural hematoma, malfunction, and any other shunt-related complication, were analyzed via Fisher’s exact test, with P
- The overall shunt-related complication rate in this study was 19%. Overall rates of infection, shunt failure, and readmission within 180 days were 3%, 11%, and 34%, respectively. No difference was seen between SC and NSC groups in any complication rate overall or on subgroup analyses.
- When comparing fixed versus programmable and flow- versus pressure-regulating valves, the latter in each analysis had significantly lower malfunction and total complication rates.
Excessive drainage of cerebrospinal fluid may result in acquired Chiari I malformation (overcrowding of the posterior fossa and tonsillar herniation). This leads to excruciating headaches, hearing loss, fatigue, muscle weakness, and loss of cerebellum function.
Slit ventricle syndrome is one more complication of ventriculoperitoneal shunt. It develops several years after the procedure and features cyclical symptoms which can be alleviated by lying prone. And finally, intraventricular hemorrhage may develop during or after the procedure. Hemorrhage may also accompany the revision of the shunt.















Your thoughts on this
Loading...