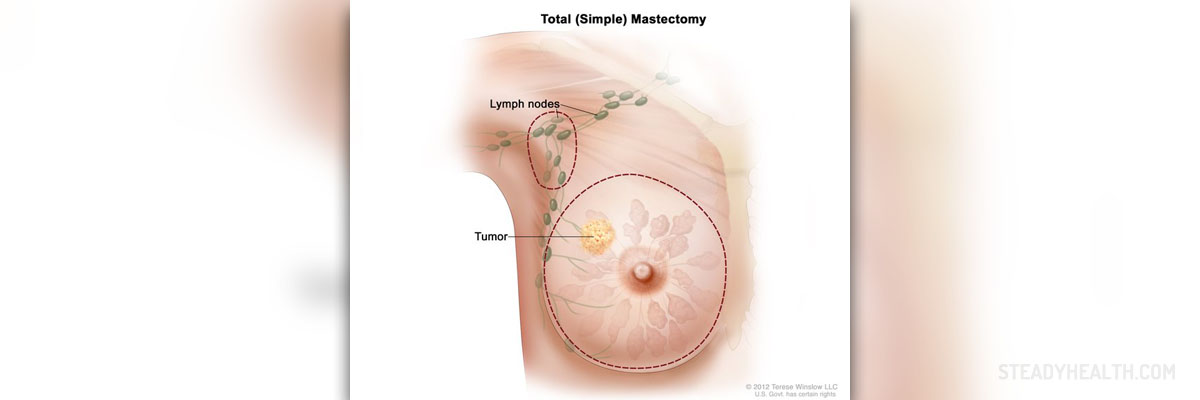
Mastectomy
Mastectomy is a surgical procedure that involves the removal of the breast. The breast is usually removed because of cancer, but in some cases, it is removed in order to prevent breast cancer. Depending on the exact position and the size of cancer, mastectomy may include the elimination of the entire breast, together with the nipples, muscles behind it, and the lymph nodes, or it can include just the tissue of the breast.Procedure
Mastectomy is performed under general anesthesia and it takes about two hours. The surgeon will make the incisions on the breast and remove the affected tissue and close the wound. After the procedure, a tube will be placed near the incision in order to drain the fluid. The tube will be removed after a couple of days. You will also be given some painkillers.
Complications
Mastectomy is considered to be a safe surgical procedure. However, there are some possible complications that may occur after mastectomy. Since it is performed after general anesthesia, you may feel sick for some time after the procedure. Further complications of the surgery include blood loss, internal bleeding, allergic reaction to the medications given to you, problems with breathing, blood clots, or heart attack. You may feel also pain in the breast, shoulder, and arm if the lymph nodes have been removed. The wound can swell due to the excess amount of fluid under the scar.
If this condition does not go away on its own after a week or two, your doctor will have to perform drainage. The wound can become infected after the surgery. The symptoms of infection include redness of the skin, pain, and swelling. Your doctor will prescribe some antibiotics for the infection. If some of the nerves have been damaged during the surgery, this can cause numbness around the wound or even in the arm. If the arm becomes swollen and you feel pain in it, it can be a result of built-up fluid. This condition is called lymphoedema and it can occur several months after mastectomy. It is important to see your doctor in case you experience any unusual changes.
Coping
After mastectomy, your physical appearance will be changed. This can be very difficult and emotional for many women who had their breasts removed. It is important for a woman to get both physical and psychological care after the surgery. At first, you can wear special bra implants, but a lot of women decide on reconstructive surgery.
- Using the claims-based MarketScan database, we described complications in 14,894 women undergoing mastectomy for breast cancer from 1998-2007 who received immediate autologous reconstruction (n=2637), immediate implant-based reconstruction (n=3007), or no reconstruction within the first two postoperative years (n=9250). We used a generalized estimating equation to evaluate associations between complications and radiotherapy over time.
- Wound complications were diagnosed within the first two postoperative years in 2.3% of patients without reconstruction, 4.4% with implants, and 9.5% with autologous reconstruction. Infection was diagnosed within the first two postoperative years in 12.7% of patients without reconstruction, 20.5% with implants, and 20.7% with autologous reconstruction.
- 5219 (35%) women received radiation. Radiation was not associated with infection in any surgical group within the first six months but was associated with an increased risk of infection in months 7-24 in all three groups. In months 7-24, radiation was associated with higher odds of implant removal in patients with implant reconstruction and fat necrosis in those with autologous reconstruction.
- Overall, slightly more than half (52.2%) of women receiving mastectomy without reconstruction were hospitalized for their index surgery; most (74.6%) of those receiving immediate implant-based reconstruction and almost all (96.0%) of those receiving immediate autologous reconstruction were hospitalized. Among those who were hospitalized, the median length of stay was 2 days for those receiving mastectomy without reconstruction and those receiving immediate implant reconstruction, and it was 5 days for those receiving immediate autologous tissue reconstruction.
- The effects of radiation therapy on the irradiated chest wall and reconstructed breast are widely feared but poorly understood. Radiation effects include acute toxicities that are generally inflammatory in nature, including soft tissue edema and skin erythema, sometimes accompanied by dry or moist desquamation of the treated skin. Late effects can include persistent skin changes, vascular compromise, and soft tissue fibrosis. In the setting of breast reconstruction, these toxicities may lead to an increased incidence of complications of the sort evaluated in this study, which may require repeated surgical interventions for correction.















Your thoughts on this
Loading...