Streptococcal infection is a rather common bacterial infection that typically affects the throat, to be more precise, the pharynx and the tonsils. It may be acute and chronic. Chronic streptococcal infection of the tonsils may cause serious damage to these organs. Tonsils have an important role in childhood. These lymphatic organs represent the first barrier against infection.
However, in case of chronic inflammation, the tissue of the tonsils is seriously damaged, so they lose their original function and may become the source of further chronic infection. People think that once they have had tonsillectomy they will no longer suffer from streptococcal infection of the throat. They are wrong since this bacterial infection may also develop even if there are no tonsils in the oral cavity.
Causes of Strep Throat
Streptococcal infection of the throat most frequently affects children and teenagers. This infection is caused by Streptococcus pyogenes (group A Streptococcus). These bacteria may represent the normal flora of the nasal and oral cavity and lead to no infection. Still, if there are favorable conditions the bacteria start to multiply rapidly and uncontrollably, causing infection.
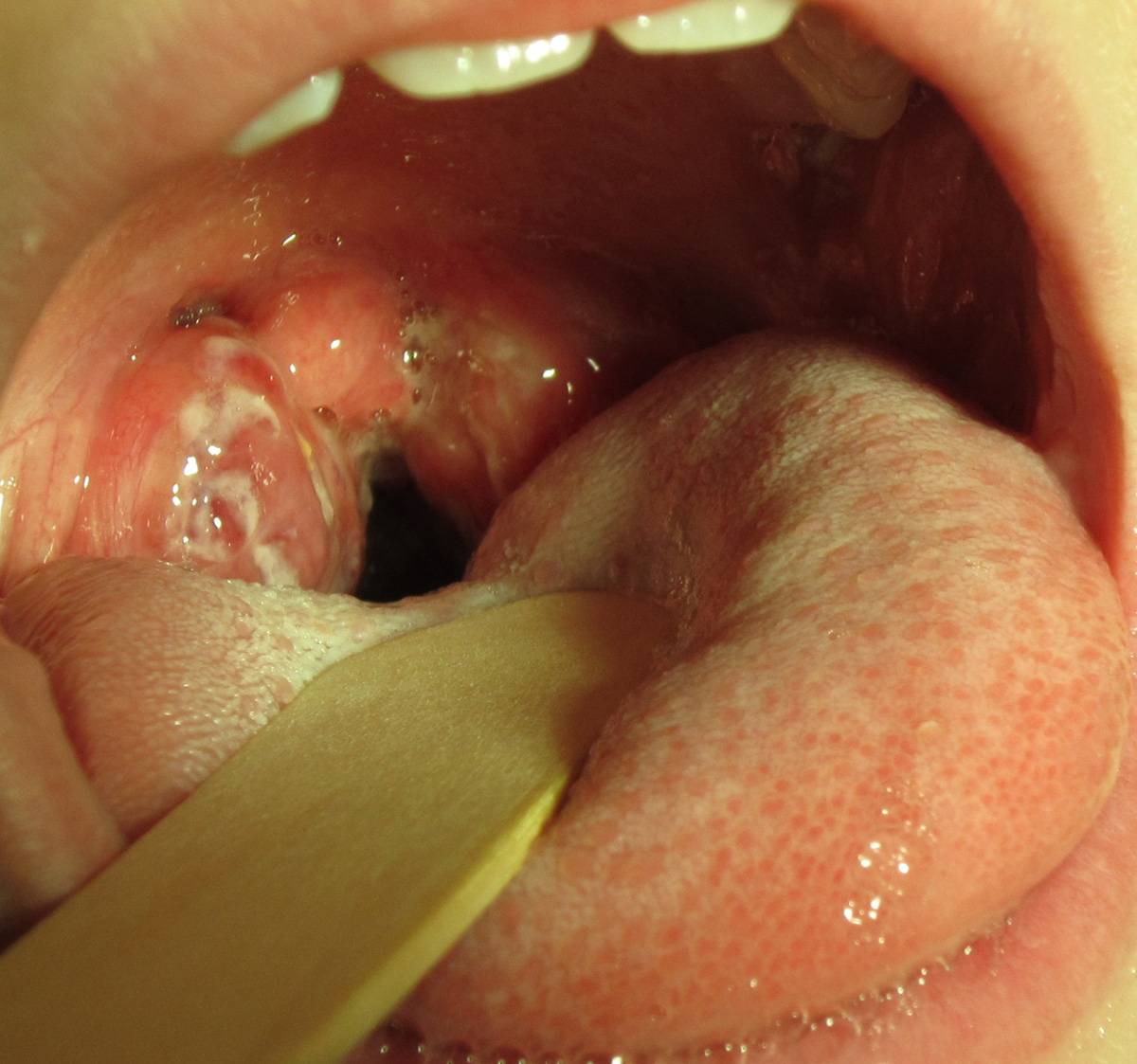
The bacteria multiply and the pus collects inside the tonsils. They become enlarged and cause swallowing difficulty and pain in the throat. Fever, cough, runny nose, and red eyes are accompanying symptoms of strep throat. In the severe form of the disease, even cervical lymph nodes may become enlarged. Physical examination of the affected tonsils reveals their enlargement and the presence of white or yellowish patches.
- Based on 2010 estimates that each year RHD caused more than 345,000 deaths added to previous estimates that Strep A invasive infection caused more than 163,000 deaths, Strep A was postulated to be the fifth most lethal pathogen in the world. Strep A vaccines could significantly reduce this disease burden. Moreover, the World Health Organization highlights the potential role of Strep A vaccines in reducing antibiotic treatment of presumed Strep A sore throat, which could plausibly lead to reduced levels of antibiotic resistance and associated harms.
- A review of the burden of Strep A diseases published in 2005 estimated that more than 616 million cases of Strep A sore throat occur globally each year. Since then, a single systematic review and meta-analysis of the incidence of sore throat and Strep A sore throat has been published, which reported a pooled Strep A sore throat incidence of 10.8 episodes per 100 child-years from six studies. Collectively, these published reviews had significant limitations.
- We used Clarivate Analytics’ Web of Science platform to search WoS core collection, PubMed, Medline, data citation index, KCI-Korean Journal Database, Russian Science Citation Index, and the SciELO Citation Index for articles published between Jan 1, 2000, and Feb 15, 2021, from any country and in any language. The risk of bias was assessed using the JBI critical appraisal checklist. We used random-effects meta-analyses to pool sore throat and Strep A sore throat incidence rates from community-based studies. Our study was registered with PROSPERO (CRD42020181103).
- Of 5,529 articles identified by the search strategy, 26 studies met the inclusion criteria, but only two included data to determine incidence among adults. The pooled incidence rate, calculated for children only, was 82.2 episodes per 100 child-years (95% CI 25.2–286.3, I2 = 100%) for sore throat (7 studies; 7,964 person years) and 22.1 episodes per 100 child-years (95% CI 14.7–33.1, I2 = 98%) for Strep A sore throat (9 studies; 15,696 person years).
- The pooled cumulative incidence rate of sore throat from five studies was 31.9 per 100 children. There was significant methodological and statistical heterogeneity among studies, and five of 26 studies had a risk of bias score less than five (range: nine [maximum score] to one).
Strep Throat without Tonsils
Once the tonsils are surgically removed they are no longer a potential source of the infection. Unfortunately, surgical resection of the tonsils does not mean that one is protected against strep throat infection for good. On the contrary, even people who have undergone tonsillectomy may again develop strep throat infection. The only difference is that people without tonsils will suffer from symptoms and signs of isolated infection of the throat.
Tonsillectomy is a good way of reducing the recurrence of strep infection. The incidence of strep throat infection in people who have undergone tonsillectomy drastically reduces.
Symptoms and signs of strep throat infection without tonsils are very similar to those if the tonsils have not been removed. Infection is contagious and can be easily spread via secretions from the nose and mouth.
A definitive diagnosis can be set thanks to throat swab culture. If the results are positive, the treatment is the same as in strep throat with tonsillitis. It includes antibiotics, gargling with warm salt water, and intake of plenty of fluids and lozenges, which may help with pain relief.
















Your thoughts on this
Loading...