Skin rash is a certain type of medical condition which is characterized by skin sores, discomfort, itching, color changes and bumps. Skin rash may also commonly affect the groin and it can be caused by rubella, roseola, measles, fifth diseases chickenpox and other sorts of so-called childhood diseases. Contact dermatitis and various different sorts of allergic reactions are among the most common causes of groin rash.
Groin Rash Causes
Seborrheic dermatitis, psoriasis and eczema may cause red scaly rashes on the groin. Tinea cruris and erythrasma may also trigger the development of brown scaly patches on the groin. Erythema nodosum, intertrigo, the Kawasaki disease and various other types of inflammatory conditions may also be held responsible for the onset of rash on the groin area. Groin rashes may also be caused by various different types of infections, and in those cases they may also be accompanied by pustules. Those who suffer from groin rash need to seek immediate medical attention because it may spread to other areas of the body and trigger a series of serious complications.
Symptoms of Groin Rash
The symptoms of groin rash largely depend on the type of underlying medical condition which causes it in the first place. The symptoms may sometimes affect other body parts. The possible symptoms may include visible eggs or small insects in pubic hair, ulcerations on the genitals, swollen lymph nodes, red eyes, rash on other areas of the body, loss of appetite, painful sensations, aches, cough, headaches, sore throat, fever, fatigue, abdominal cramping and abdominal pain. Other possible symptoms which may accompany groin rash include swelling, redness of the soles and the palms, redness of the lips, peeling skin, nausea, vomiting, hair loss, diarrhea and changes in the appearance of the tongue. There are also certain symptoms which may indicate a potentially life threatening medical condition and those include high fever, changes in the mental status, delusions, hallucinations, lethargy, delirium, confusion, sudden behavior changes, unresponsiveness, passing out and changed levels of consciousness or alertness.
What Else Can Cause Groin Rash?
There are certain infectious types of causes of groin rash and those include tinea cruris, syphilis, shingles, scabies, phthirus pubis, mollluscum contagiosum, HIV, erythrasma, rubella, roseola, measles, fifth disease and chickenpox. Other common causes of groin rash may or may not include seborrheic dermatitis, psoriasis, Kawasaki disease, intertrigo, erythema nodosum, eczema, contact dermatitis and various different types of allergic reactions. Groin rash may be associated with dangerous medical conditions such as Fournier’s gangrene and meningococcal meningitis.
- Tinea cruris is caused by dermatophytes belonging to three genera, Trichophyton, Epidermophyton, and Microsporum.
- Several risk factors have been identified that predispose an individual to tinea cruris, including excessive perspiration, occlusive clothing, improper hygiene, diabetes mellitus, immunocompromise, and lower socioeconomic status.
- Cutaneous mycoses, including tinea cruris, affect 20 to 25 percent of the world's population.
- Developing and tropical countries have an increased prevalence of dermatophyte infections secondary to high temperatures and increased humidity. In the United States, there have been an estimated 29.4 million cases of superficial fungal infections and over 51 million reported physician visits. Adolescent and adult males comprise the majority of patients seen for tinea cruris and are affected by the disorder with increased frequency. Worldwide increases in the occurrence of dermatophytoses and the discovery of recalcitrant infections have caused global concern.
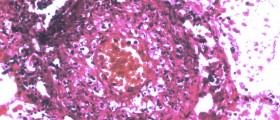
- In most cases, tinea cruris can be diagnosed clinically; however, several tests exist to investigate a rash of the groin with unknown etiology. Potassium hydroxide (KOH) preparations, skin biopsy with periodic acid-Schiff (PAS) stain, and fungal cultures on Sabouraud’s agar media can be utilized when the diagnosis is in question or the case of recurrent or recalcitrant episodes.
- Antifungals utilized in treating dermatophytoses, including tinea cruris, target the synthesis of ergosterol, a vital component of fungal plasma membranes. Management strategies are similar worldwide; however, some countries have specific guidelines based on their region's fungal profile. Topical therapies are effective and usually preferred. Allylamines (terbinafine, butenafine, naftifine) and azoles (clotrimazole, miconazole, sulconazole, oxiconazole, econazole, ketoconazole) are the mainstays of topical treatment regimens. They are generally prescribed once or twice daily for two to four weeks.
- Failure of therapy and recurrence are the most likely complications of tinea cruris. They have been attributed to reinfection from close contacts, autoinfection from separate body locations, infection by uncommon species such as zoonoses, misdiagnosis, drug resistance, and non-adherence to the management plan. Steroid use may suppress the physical signs of tinea cruris, making the diagnosis more difficult.

















Your thoughts on this
Loading...