Apoplexy: A Sudden Neurological Impairment
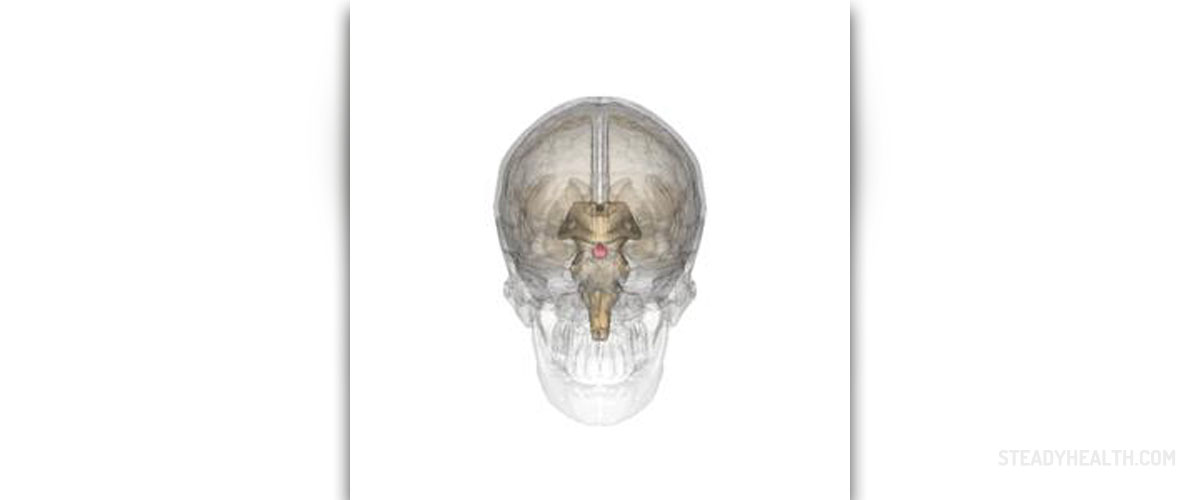
The term apoplexy refers to sudden impairment of neurological function that basically occurs due to some kind of cerebral hemorrhage. In case of pituitary apoplexy there is bleeding into the pituitary gland, a tiny little organ located in the skull, to be more precise at the base of the brain in a small bone cavity called the sella turcica.
In the majority of patients such bleeding is closely connected with a tumor of the pituitary gland. Many times bleeding triggers a sudden headache and rapid progression of vision impairment in the form of visual field defects or double vision. Additionally, since the gland plays significant role in synthesis of a range of hormones, pituitary apoplexy is a reason why a person may suddenly experience different hormone imbalances.
Pituitary Apoplexy Characterized by Headache
As it has already been mentioned pituitary tumors are the most reported underlying cause of pituitary apoplexy. However, the bleeding of this type is also reported to occur even though there is no tumors affecting the gland. The very characteristics of vascularisation of the pituitary gland, especially its anterior part, make the gland susceptible to bleeding. In patients in whom there is a pituitary gland, the bleeding may begin once some blood vessels of the tumor open spontaneously or if the tumor is malignant and penetrates the previously healthy blood vessels of the gland.
Statistical data show that pituitary apoplexy affects 1.5 -27.7% of patients with pituitary adenomas. The bleeding is more reported in men and is common in individuals between 37 and 57 years of age.
Clinical presentation is associated with headache in almost all cases. As a matter of fact headache is reported in approximately 95% of all patients. Headache is sudden and may be unbearable. It develops as a result of stretching of the dura mater or irritation of the 5th cranial nerve (trigeminal nerve). Initially, the pain remains localized on one side of the head and is mostly felt behind the eyeballs. Eventually, it spreads to the entire cranium.
Furthermore, patients experience nausea and start to vomit. These two characteristics are closely connected with increased intracranial pressure as well as irritation of the brain's membranes.
One more frequent complaint of such patients is visual impairment. Namely, visual acuity defects occur in 52% of patients while 64% of them report visual field defects. These issues develop as a consequence of compression of the optic chiasm, optic tract or the very optic nerve by the tumor or the accumulated blood. The blood may also collect inside these structures and trigger the same symptoms/signs. Ocular paresis is a complication of pituitary apoplexy. It develops due to compression of the cavernous sinus and nearby cranial nerves (the 3rd, 4th and 6th cranial nerve).
Some patients additionally develop Horner's syndrome. It is also possible that one will end with hemispheric deficits, compression of the carotid sinus or leakage of blood into the subarachnoid space which subsequently triggers meningismus, stupor and finally coma.
If bleeding additionally affects the hypothalamus, the patients may suffer from thermal regulation impairment.
The examination of samples of cerebrospinal fluid obtained by performing a spinal tap confirms increased pressure and pleocytosis as well as increased number of erythrocytes and xanthochromia.
And finally, severe destruction of the tissue of the pituitary gland leads to various endocrinologic deficiencies.
Pituitary Apoplexy - Treatment Options
Initially, as soon as the condition is confirmed the goal of the treatment is to stop the bleeding and stabilize the circulatory system. Severe cases require hospitalization. These patients are admitted to a high dependency unit.
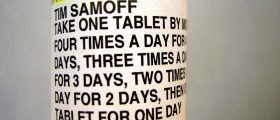
In case there is acute adrenal deficiency (a potentially lethal complication of pituitary apoplexy), patients are administered saline and dextrose solutions intravenously. The amount of solutions depends on the age of the patient. Furthermore, such patients receive intravenous or intramuscular Hydrocortisone injections.
After patients have been stabilized doctor determine whether there is possibility and a need to perform surgical decompression of the pituitary gland. Patients with severe visual loss and visual field defects undergo surgery. Other candidates for the surgery are those with significantly reduced level of consciousness. In the majority of cases patients undergo transphenoidal surgical approach, without having their cranium opened. This approach includes insertion of surgical instruments through the nose towards the sphenoid bone. The bone is opened and the gland is finally reached. This is very successful surgery and may improve vision considerably, especially if performed within a short period of time after pituitary apoplexy.
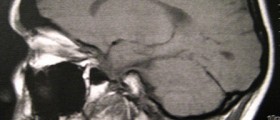
After recovery all patients have regular check-ups and are monitored by a well experienced endocrinologist who can timely diagnose any hormonal imbalance that may eventually occur. It is also important to perform MRI scans 3-6 month after the initial bleeding and repeat this once per year.
As far as prognosis is concerned, it has become much better since steroid replacement was introduced. The outcome is also good if patients are operated on time. The prognosis is worse in those who cannot undergo surgery because of their general health.













Your thoughts on this
Loading...