What is Malassezia
Malassezia is a genus of fungi or yeasts, normally living on the human skin. There are about the 10 types of this yeast and they cause Pityriasis versicolor, Pityriasis folliculitis, seborrhoeic dermatitis and dandruff. Babies and adults on the lipid substitution therapy also have these fungi in the blood.
Disorders
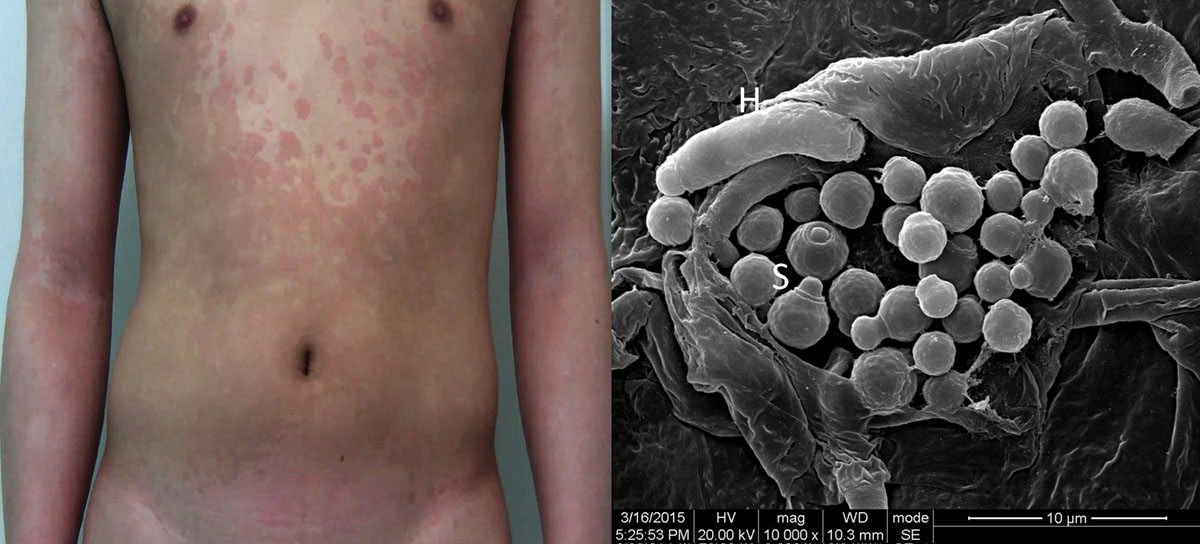
Pityriasis versicolor is a condition when skin becomes hyper or hypo-pigmented. Malassezia cause fungal infection of the skin and leads to skin lesions, visible as white, pink or brown patches, covered with dry skin that looks like dandruff. Most lesions appear on the upper body, arms and shoulders, and rarely affect neck or face. Caucasians experience hyper pigmentation and Aborigine in Australia hypo pigmentation. Skin changes are visible under the ultraviolet (UV) light and they have greenish fluorescence.
Pityriasis folliculitis appears as bumps and pimples on the chest, upper arms or the back. Rarely, this skin changes happen on the neck or the face. They are often connected to the exposure to the sun. The condition is usually treated with imidazole creams, but some cases require oral anti-fungal medications, like ketoconazole or itraconazole. Doctors also recommend prophylactic therapy.
Risk Factors
Dandruff and seborrhoeic dermatitis are usually caused by Malassezia furfur (M.furfur). There are some risk factors associated with these disorders, like genetics, sebum and skin changes, occlusions and also emotional factors. Patients suffering from AIDS or Parkinson’s disease are also quite often infected with these fungi. These conditions appear as red lesions and scaling on the scalp, face, eyebrows or ears, and might spread to upper body. Therapy includes imidazole or ketoconazole locally. Most cases need re-treatments.
- Currently, the genus comprises 18 lipid-dependent species with a variable distribution on different hosts and pathologies. Additionally, by using both fingerprinting methods and multigene sequence analysis, different Malassezia genotypes were identified as strictly related to the host, geographical origin, and/or clinical manifestations
- Since the designation of the genus Malassezia by Baillon in 1889, the taxonomy has been updated and currently the genus comprises 18 lipid-dependent species with different genotypes showing variable pathology and distribution on different hosts. All Malassezia species are lipid-dependent and, with the exception of Malassezia pachydermatis, do not grow on Sabouraud Dextrose Agar (SDA), which is most commonly used for culturing fungi in clinical labs.
- Based on a phylogenomics study using 164 core eukaryotic genes, three main clusters were identified: Cluster A consisting of M. furfur, M. japonica, M. obtusa, and M. yamatoensis; Sub-cluster B1, with the most abundant human skin inhabitants M. globosa and M. restricta; Sub-cluster B2 consisting of M. sympodialis, M. dermatis, M. caprae, M. equina, M. nana, and M. pachydermatis; and Cluster C forming a basal lineage with M. cuniculi and M. slooffiae. Four more species have been described since then: M. brasiliensis and M. psittaci from parrot, M. arunalokei from human scalp, and M. vespertilionis from bat. Multiple genotypes of a species can colonize the same patient, but some genetic types might be linked to a particular body site or pathology thus indicating an affiliation of Malassezia genotypes with host, geographical origin and/or clinical manifestations
- Malassezia furfur, M. sympodialis, and M. pachydermatis are the only Malassezia species isolated from bloodstream infections to date. Some authors propose that the fungal density on the skin as well the host immunological competence might be driving factors influencing their pathogenic role. Malassezia bloodstream infections have been described in adult and child immunocompromised patients, and neonates. According to general knowledge, the main ecological niche of Malassezia yeasts is human and animal skin, and they represent 50 to 80% of the total human skin mycobiome. Therefore, it would make sense to consider the skin mycobiome as a potential reservoir and point d'entrée for bloodstream infections.
- Clinical features, laboratory markers, strategies of patient management, and outcomes of Candida and Malassezia fungemia do not differ. In some studies, M. furfur fungemia appeared earlier than candidaemia (average day 26 vs. day 42), most likely due to its exogenous origin. In addition, duration of Malassezia fungemia is longer than candidaemia, most likely due to the late removal of the central venous catheters (CVC) and also as a result of the lower efficacy of the antifungal therapy. The first signs causing suspicion of Malassezia fungemia usually are bloodstream infections manifested in fever of unknown origin in hospitalized and severely immunocompromised patients with CVC (i.e., preterm neonates or cancer patients) or in patients with pulmonary distress.
People using catheter or those on the lipid replacement treatment may be affected by fungaemia.
Diagnosis
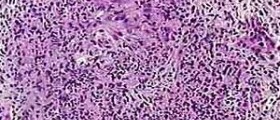
Skin scrapings, blood and catheter culture are commonly used to diagnose these fungi. Using a microscope, laboratory can identify the specific M.furfur characteristics and identify the fungus. In the cases of suspected fungaemia, it is usually necessary to cultivate culture preparations.
Anti- fungal Treatment
Pityriasis versicolor is treated with imidazole solution or some other local preparation, and sometimes ketoconazole shampoo. Shampoos with zinc pirithione and selenium sulfide lotion have also been proven helpful in this condition. Widespread lesions need oral treatment with ketoconazole or itraconazole.
Skin pigmentation get back to normal after the treatment, but it needs time to heal, sometimes even several months. Because the relapses are common for this type of disorder, prophylactic use of local preparations is necessary. Usually, use of the preparation one or two time per week is enough.
















Your thoughts on this
Loading...