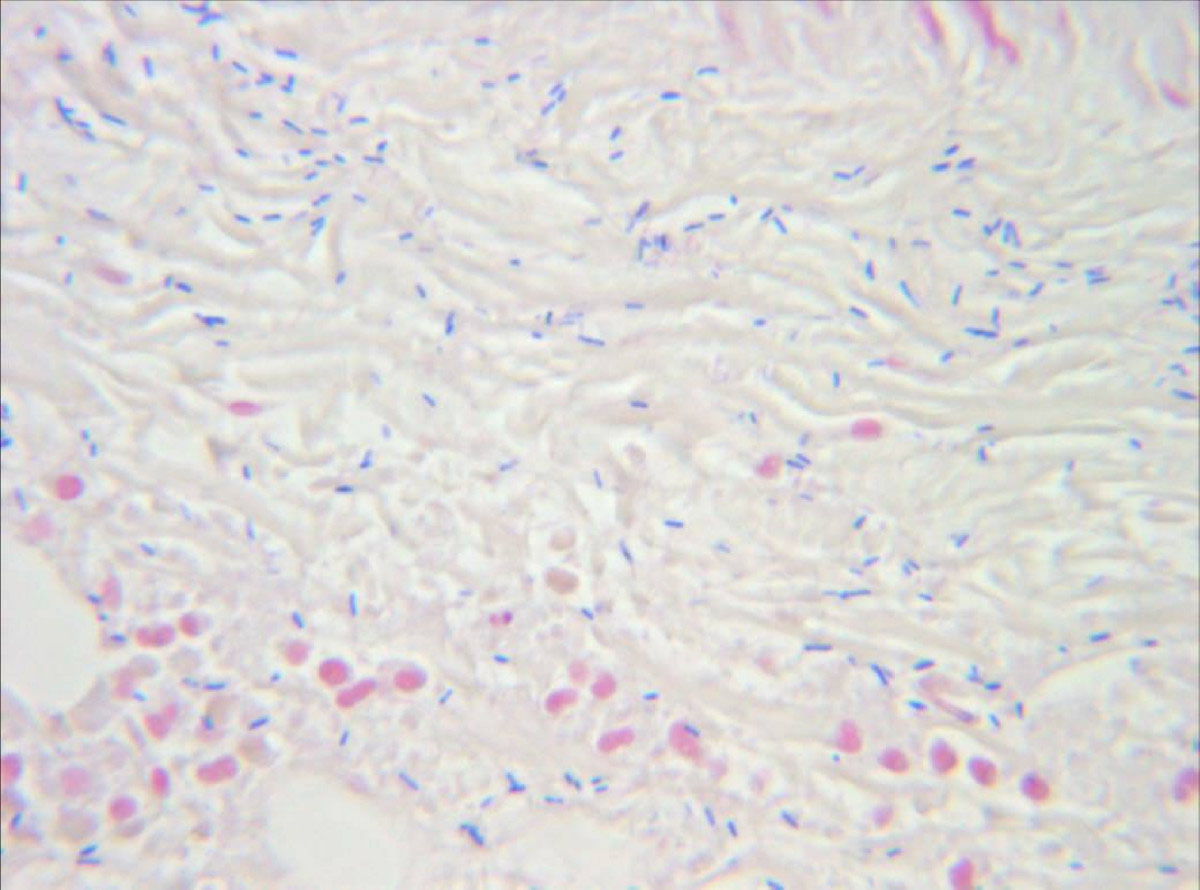
Necrotizing fasciitis is a form of bacterial infection where skin and deeper subcutaneous tissues such as fascia are affected. The process is rather rapid and the involved tissue finally ends up necrotic. The depth of the subcutaneous layer is what determines the speed of the disease spreading. This condition can be caused by previous trauma or foreign bodies present in the surgical wound. Sometimes there is no evident cause so it is classified as idiopathic necrotizing fasciitis. Different kinds of bacteria can lead to the state. They include both aerobic and anaerobic bacteria as well as the combination of these two types. If anaerobic bacteria lead to this severe infection they cause a gas production which may be visualized on radiographs. Necrotizing fasciitis is pretty hard to be diagnosed in the early stage and it tends to progress quickly. The treatment is aggressive and must be conducted on time.
Most cases of necrotizing fasciitis include both aerobic and anaerobic bacteria. Hypoxia is suitable place for bacterial multiplication especially since the function of specific leukocytes called polymorphonuclears is reduced in conditions of decreased oxygen supply. The initiators of the condition are mainly group A hemolytic streptococci and Staphylococcus aureus. Other bacteria such as Bacteroides, Clostridium, Enterobacteriaceae, Proteus, Pseudomonas and Klebsiela may be involved as well.
All the patients are treated aggressively. In case of inappropriate respiration patients are intubated and supplied with the oxygen. In order for medications to be administered an I.V. line is opened but not on the affected extremity. Solutions such as Lactated Ringer are administered. Heart function is closely monitored. In case of hypovolemia (decreased volume of the blood) the patients are inserted urinary catheter to monitor the urine production and excretion. The most important thing is to start with antibiotics immediately. The methods that are essential in treatment of this severe disease include surgical debridement which is the excision of the damaged and infected tissue. This can prevent disease from spreading. As the disease leads to huge wounds and destruction of subcutaneous tissue an option is hyperbaric oxygen treatment. In most severe cases a patient might end with the amputation of the destroyed body part.
In case of infections caused by Streptococci patient is given Penicillin G (and Clindamycin as an alternative). Both groups of aerobic and anaerobic bacteria must be covered. This can be done by Gentamicin in a combination with Clindamycin or Chloramphenicol. Even a combination of Metronidazole and the third generation of Cephalosporins is an option.















Your thoughts on this
Loading...