Group B Streptococcus screening and testing is a normal, routine part of prenatal care in the United States. Pregnant women will normally be tested at some point during their third trimester of pregnancy, and if they are found to have been colonized by GBS, steps for treatment will be undertaken. Why? GBS infections can cause babies to become seriously ill. About two percent of infants who were infected with GBS get sick. Early onset GBS leads to fever, lethargy and sometimes breathing difficulties. And late onset Group B Strep causes respiratory infections, and sometimes seizures as well.
GBS is treated with antibiotics, but because research found that antibiotic treatment of Group B Strep is not very effective in pregnancy, the main treatment of the bacterium actually takes place during labor. In the United States, those laboring women who are GBS+ will be given IV antibiotics when they check in to the hospital. This prevents transmission to the baby while the mother gives birth. Women whose GBS status is unknown when they go into labor will be administered IV antibiotics just in case they are GBS positive.
- www.cdc.gov/groupbstrep/about/prevention.html
- www.cdc.gov/features/groupbstrep/index.html
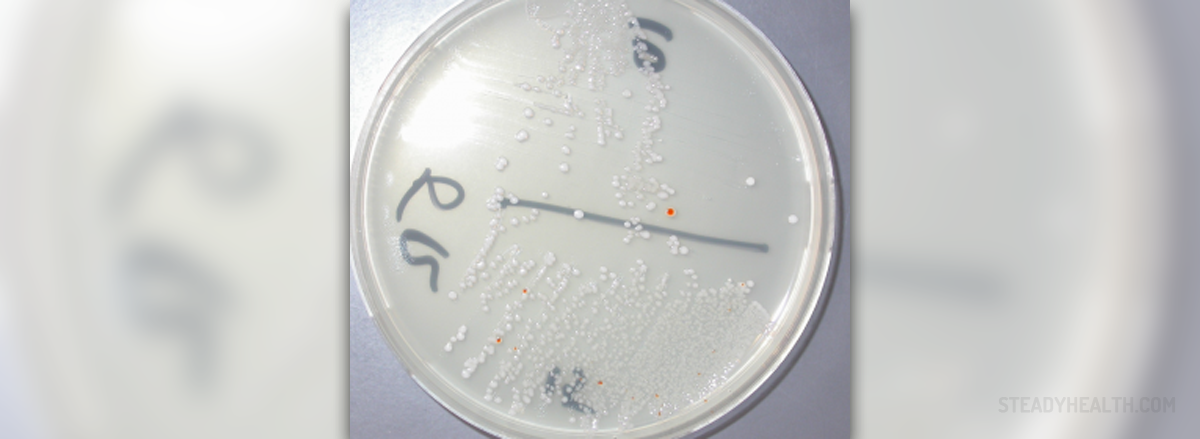
- Photo courtesy of 43trevenque by Wikimedia Commons: en.wikipedia.org/wiki/Group_B_streptococcal_infection#/media/File:S_agalactiae_vagino-rectal_culture_GRANADA.png















Your thoughts on this
Loading...