Lung Cancer and the Surgery as a Method of Treatment
When it comes to cancer deaths in the United States, lung cancer as one of the most serious types of cancer, is the leading cause. The greatest number of cases is caused by smoking, because those who smoke, as well as those who are exposed to secondhand smoke, are at the highest risk of developing lung cancer.
There are two types of it, small cell lung cancer, which is practically typical of heavy smokers, and non-small cell lung cancer, which includes squamous cell carcinoma, adenocarcinoma, and large cell carcinoma.
As for the treatment, the sooner the cancer is diagnosed, the better the chances for successful treatment are. Several options are available, but which will be chosen depends mostly on the type and location of the cancer, the stage at which it is diagnosed, and the general health of the patient. Surgery, radiation therapy, chemotherapy, and targeted drug therapy are the most efficient methods, but very frequently the treatment requires the combination of at least two methods.
Surgery procedures that can be done in such cases are wedge or segmental resection, both requiring the removal of either a smaller or larger portion of the lung and the margin of the healthy tissue; lobectomy, in which an entire lobe of the lung has to be removed; and pneumonectomy, in which the whole lung has to be removed.
Possible Complications After Lung Cancer Surgery
Having in mind the seriousness of the condition in question, the surgery is also one of the more serious procedures, and it carries a significant amount of risk of possible complications. What can go wrong during or after the surgery involves bleeding, infection, blood clots, and collapse of the lung or a part of the lung, but it is also not excluded that the nearby structures and tissue, or even the heart may be damaged.
Such complications may even be life-threatening and may have fatal consequences for a patient. The risk of anesthesia is also always present, and although anesthesiologists take measures of precaution to reduce these possibilities to the minimum, it is never possible to exclude them entirely.
After lung cancer surgery of any kind, the patient will have to face pain in the chest wall and shortness of breath, but these are practically inevitable symptoms, and they will gradually disappear, so they cannot be considered complications.
- Clinical data of 956 patients with NSCLC were analyzed. Patient factors such as sex, age, comorbidities, smoking history, respiratory function, and the lobe involved in lung cancer and operative factors such as operative approach and operative procedures were collected and analyzed.
- Male sex (odds ratio [OR]: 1.73, 95% confidence interval [CI]: 1.09–2.75, p?=?0.01), coexistence of asthma (OR 2.68, 95% CI 1.19–6.02, p?=?0.01), low percentage of forced expiratory volume in 1 s (FEV1) (OR 1.41, 95% CI 1.02–1.95, p?=?0.03), and lobectomy or greater resection (OR 2.47, 95% CI 1.66–3.68, p?0.01) were identified as significant risk factors for postoperative complications. Male sex (OR 1.98; 95% CI 1.03–3.81, p?=?0.03) and complete video-assisted thoracic surgery and robot-assisted thoracic surgery (OR 1.64; 95% CI 1.09–2.45; p?=?0.01) were identified as significant risk factors for postoperative air leakage.
- Coexistence of asthma (OR 9.97; 95% CI 3.66–27.38; p?0.01) was identified as a significant risk factor for postoperative atelectasis or pneumonia. Lobectomy or greater resection (OR 19.71; 95% CI 2.70–143.57; p?0.01) was identified as a significant risk factor for postoperative arrhythmia.
- www.nhs.uk/conditions/lung-cancer/treatment/
- www.nhs.uk/conditions/lung-cancer/
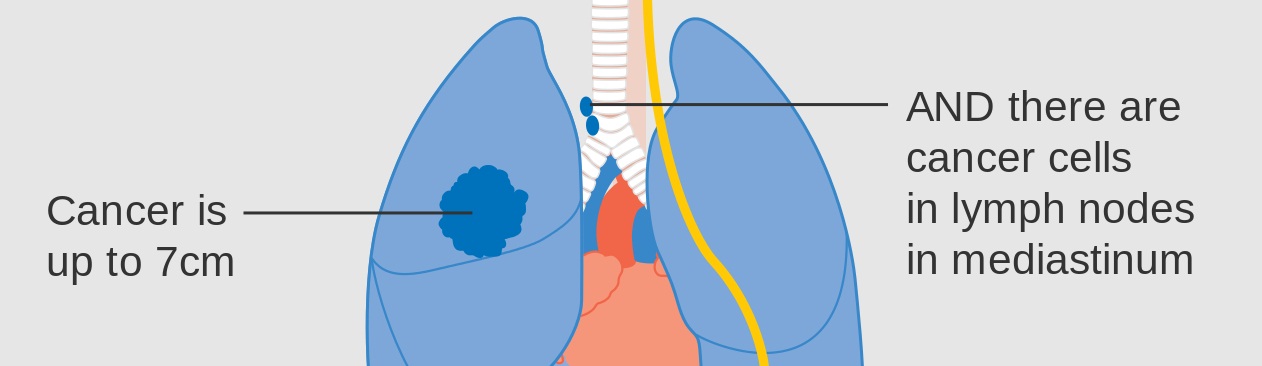
- Photo courtesy of Cancer Research UK by Wikimedia Commons: commons.wikimedia.org/wiki/File:Diagram_1_of_3_showing_stage_3A_lung_cancer_CRUK_008.svg















Your thoughts on this
Loading...