Inclusion body myositis is a medical condition affecting various muscles, causing their inflammation and subsequent weakness, atrophy and wasting. The condition is chronic and progressive, affecting both proximal and distal muscles. The signs of muscle wasting are most prominent on both, the upper and lower extremities.
Classification of Inclusion body myositis
Inclusion body myositis may develop in the form of sporadic disease of hereditary inclusion body myopathy.
As for sporadic inclusion body myositis, the disease typically leads to destruction of muscle cells due to autoimmune process as well as degeneration that occurs at the same time. The affected muscles cells are damaged and their anatomical features are radically changed which affect functions of the muscle, decreasing its strength and the overall performance. Sporadic form of the disease, as the very name suggests, affects people randomly.
Scientists managed to identify several not so common forms of hereditary inclusion body myopathies. They develop as a consequence of effective genes that are inherited from parents. The inheritance varies and is either autosomal dominant or autosomal recessive.
Finally, there is one more type of the condition that has been identified in several families, affecting multiple siblings in the same generation. This is the so called familiar inflammatory sporadic inclusion body myositis. This medical condition has nothing to do with gene transmission.
When it comes to symptoms and signs of this disease most patients experience different set of medical issues. The condition itself is disabling, affecting patient's mobility in the long run. Namely, the damaged muscles waste away, lose their strength and become atrophic. This makes patients incapable of performing different activities such as lifting or even holding objects, bending, reaching for different items, etc. Most patients additionally develop problems with balance and posture. They become prone to falls, a variety of injuries and additional health problems. Eventually, all patients require aids like a cane, a walker and in the most severe cases a wheelchair.
Apart from affecting muscles necessary for mobility, inclusion body myositis also affect muscles one uses for chewing and swallowing. As a result patients become unable to swallow food and may easily develop aspiration pneumonia, inflammation of the lungs that occurs once the food enters the airways instead of being transferred into the stomach. Swallowing difficulty, medically known as dysphagia is reported in 40-85 % of patients suffering from the disease.
As far as causes of inclusion body myositis are concerned, these have not been identified yet even though many experts believe that the condition develops due to a combination of genetic and different environmental factors. There are two theories related to inclusion body myositis. According to the first theory, the condition is associated with an abnormal immune reaction of the body triggered by some virus. However, inadequate response to immunotherapy does not support this theory. The second theory is based on the effects of the aging process. It seems that inclusion body myositis may be degenerative in origin, connected with aging of muscle fibers due to accumulation of certain pathogenic proteins. Hopefully, one day, the actual cause of inclusion body myositis will be revealed.
Diagnosis of Inclusion body myositis
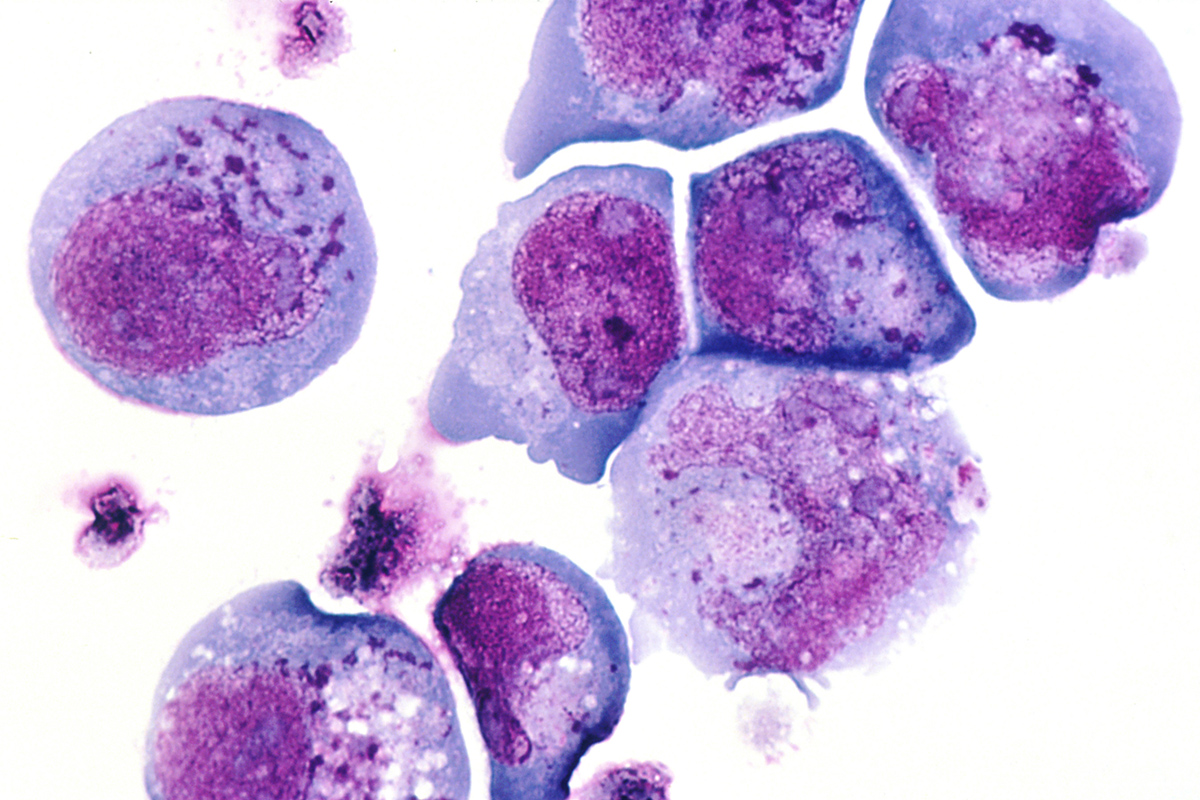
Patients basically turn to their doctors once the symptoms and signs associated with muscle weakness occur. Apart from physical and neurological exam, doctors perform several more tests and exams. For instance, such patients have increased creatine kinase CK levels, which can be confirmed by taking blood samples. The reduced strength and damage to certain muscles are confirmed with electromyography. Nevertheless, all patients eventually undergo biopsy. Pathohistological examination of taken samples definitely confirms the condition. The affected muscle cells show signs of inflammation, vacuolar degeneration and inclusions of abnormal proteins. Only a well-experienced pathologist may be certain that the person is suffering from inclusion body myositis.
Differential diagnosis includes polymyositis as well as other forms of muscular dystrophy. These can be also be ruled out after biopsy of the affected muscles.
Treatment of Inclusion body myositis
Since there is no identified underlying cause of the disease, there is no cure for it. The disease is progressive and patients may only benefit from symptomatic treatment. The goal of therapy is to relieve current symptoms and try to decelerate the progression of muscle atrophy.
There are many different medication these patients can be prescribed. Some respond well to anti-inflammatory drugs while others require immunosupressants or immunomodulatory agents. Patients also undergo a specially designed exercise plan.
It is essential to prevent falls, aspiration of food and help patients remain as much movable as they can. For instance, severe dysphagia and subsequent aspiration of food is dealt with cricopharyngeal myotomy or placement of a gastrostomy tube.
Relevant Data
It is estimated that sporadic inclusion body myositis actually accounts for the majority of cases of inflammatory myopathy among people older than 50 years of age. The course of the disease is in most cases slow. Patients with early onset of inclusion body myositis may have even a slower rate of progression.
All in all, the disease is reported to occur more in older individuals and inevitably leads to lethal outcome.
















Your thoughts on this
Loading...