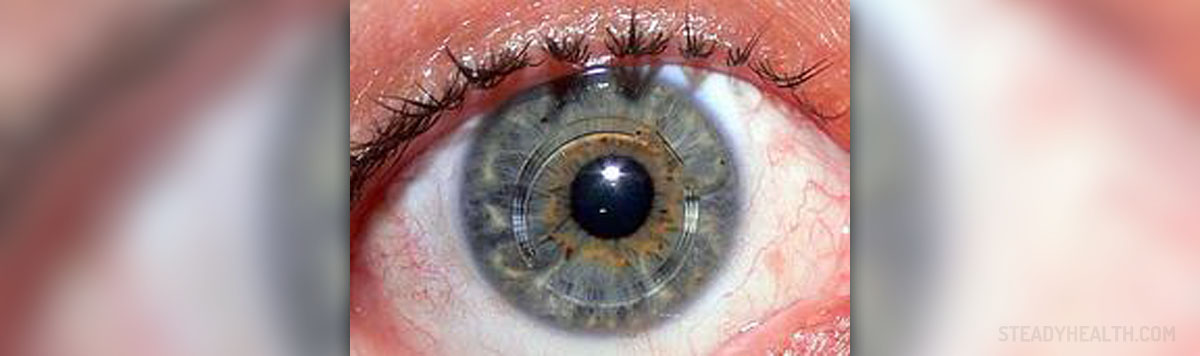
Keratoconus is a problem associated with the cornea of the eye and in 90% of cases it affects both patients’ eyes. Human cornea is normally clear and of regular spherical shape. It comprises many layers and these layers are cross-linked with collagen. Keratoconus causes loss of collagen and progressive thinning and stretching of the cornea, leading to distortion and irregular shape of this part of the eye.
Risk factors for development of this condition include rubbing of the eyes, ocular allergies, long term wear of rigid contact lenses and genetic predisposition to keratoconus. Also, people having a close relative suffering from this corneal problem are also much more likely to develop keratoconus themselves. If you have someone in the family with keratoconus, you have 50% chances to suffer from the same problem. Your sex does not play the part here, because both men and women may experience such problem with their eyes.
Keratoconus and Its Symptoms
Patients develop astigmatism and shortsightedness (myopia) as well as severely blurred vision. They cannot read or drive a car because of this problem and further progression of the disease definitively leads to even more complex health issues.
Early signs usually resemble problems of people who need to wear eyeglasses, but vision deteriorates and patients become unable to see normally from any distance. The eye or eyes affected by this condition may become itchy, red and sensitive to bright light (photophobia) or even strained because of squinting associated with an attempt to read. However, just a small percent of keratoconus patients suffer from pain.Diagnosis and Treatment Options for Keratoconus
To diagnose whether you are suffering from keratoconus or not you need to visit an eye specialist – an ophthalmologist. He or she will perform detailed eye examination and corneal topography in order to establish proper diagnosis and avoid mistaking this problem for some other condition. By using topography, the doctor may identify some visible scarring or distortion of the cornea in patients suffering from keratoconus and specifically steep curvature (around or below the center of the cornea of the eye). An ophthalmologist will be able to tell the degree and extent of this corneal deformation, concluding the progression of keratoconus.
Treatment for mild keratoconus includes reduction or elimination of shortsightedness and astigmatism, meaning that as temporary solution patients may wear contact lenses. However, there is also a new treatment called corneal collagen crosslinking with riboflavin, which should permanently resolve all problems a patient with keratoconus might have.















Your thoughts on this
Loading...