Main concern of doctors treating the patient suffering from acute tubular necrosis (usually shortened as ATN) is to prevent any further damage to the kidneys. In general, treatment consists of extracellular fluid (ECF) assessment and timely repletion of existing deficits. Patients receiving drugs toxic to the kidneys (nephrotoxic) should stop using these. In these patients, the recommendation is the same for any of the drugs eliminated by the kidneys – quick cessation is advised by most doctors.
How to Treat Acute Tubular Necrosis?
Acute tubular necrosis is usually treated by correction of oliguria, dialysis, elimination of nephrotoxins, and some dietary measures. Doctors will try to increase urine output using diuretic drugs like intravenous (IV) loop diuretics. This method is recommended only in patients whose ECF and cardiac function are found to be adequate.
A single high dose of bumetanide or furosemide (100 to 200mg) is commonly used to correct oliguria in these patients, but it usually doesn’t change anything for the patients. If they don’t improve the problem, loop diuretics should be stopped. Some doctors also used dopamine, but this is not recommended by modern medical practice, for it had no effects.
Early dialysis may be beneficial for ATN patients and hemodialysis is currently the standard treatment for serious acute kidney injury. However, some studies show that this procedure has no positive effects on recovery or survival. Continuous hemodialysis is recommended for patients suffering from hemodynamic instability or multi-organ failure.
Cessation of nephrotoxic substances should prevent further kidney damage. Elimination of nephrotoxins – Cyclosporine may benefit from calcium channel blockers. This measure may cause hypotension, and doctors avoid using it.
Dietary measures in form or adequate intake of proteins and calories can improve survival rate in ATN patients.
- Data sources: MEDLINE search for all clinical studies of therapies for ATN, supplemented by a review of the references of the identified articles.
- Study selection: Prospective studies and major retrospective studies evaluating therapies for ATN.
- Data extraction: Data on the study sample, interventions performed, results, side effects, and duration of follow-up.
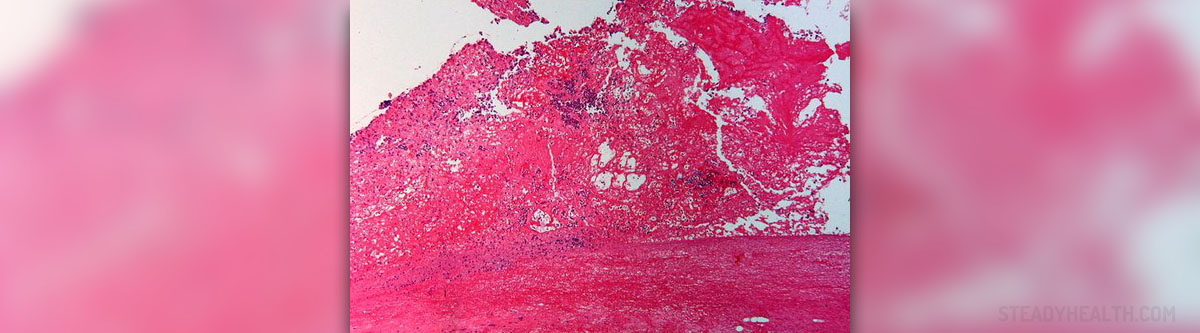
- Early diagnosis of ATN by exclusion of prerenal and postrenal causes of acute renal failure, examination of urinary sediment, and analysis of urine measures (for example, fractional excretion of sodium in the absence of diuretics) can allow the early involvement of nephrologists and improve survival.
- Enteral rather than parenteral hyperalimentation in severely malnourished patients may improve survival.
- Sepsis causes 30% to 70% of deaths in patients with ATN; therefore, avoidance of intravenous lines, bladder catheters, and respirators is recommended. Because septic patients are vasodilated, large volumes of administered fluid accumulate in the lung interstitium of these patients. This condition necessitates ventilatory support, which when prolonged leads to acute respiratory distress syndrome, multiorgan failure, and increased mortality. More aggressive dialysis (for example, given daily) with biocompatible membranes may improve survival in some patients with acute renal failure.
ATN Prevention Methods
Acute tubular necrosis may be ischemic or nephrotoxic, and these problems require a different approach when it comes to prevention. Ischemic ATN is prevented by optimizing cardiovascular function and maintenance of intravascular volume. Doctors should be especially careful when prescribing nephrotoxic drugs or afterload reducers to these patients.
Nephrotoxic ATN may be prevented with careful nephrotoxin consideration. Aminoglycosides, amphotericin B, tacrolimus, cisplatin, and Cyclosporine are known to cause nephrotoxic acute tubular necrosis in some patients. One daily dose of aminoglycosides is discovered to be less likely to cause nephrotoxic effects than the same drug given three times per day.
Lipid formulations of amphotericin B, such as colloid dispersion of this drug, complex or liposomal amphotericin B, should be less toxic for the kidneys. Reduction of the therapeutic dose is usually sufficient to reverse kidney damage due to the use of tacrolimus or Cyclosporine. Cisplatine can be less nephrotoxic if used with saline or amifostine, while some doctors recommend switching to carboplatin, considering it to be less toxic for the kidneys.















Your thoughts on this
Loading...