Renal Syndromes
Glomerulonephritis, inflammation of the glomerulus of the kidneys (the beginning component of nephrons in the vertebrate kidney), was first described as a condition in 1927. Poststreptococcal acute glomerulonephritis, which is the archetype of acute form of the disease, together with acute nephritis syndrome belongs to a group of renal syndromes. Renal syndromes all represent a set of renal diseases that are closely connected with an immunologic mechanism which precipitates inflammation and proliferation of the glomeruli. The changes resulting from the process of inflammation and accompanied proliferation might cause severe damage to other parts of the kidney as well. Basically, all the diseases of this type are responsible for reduction in urine output (oliguria) or complete cessation of urine excretion (anuria). There is also back pain and the blood in urine.
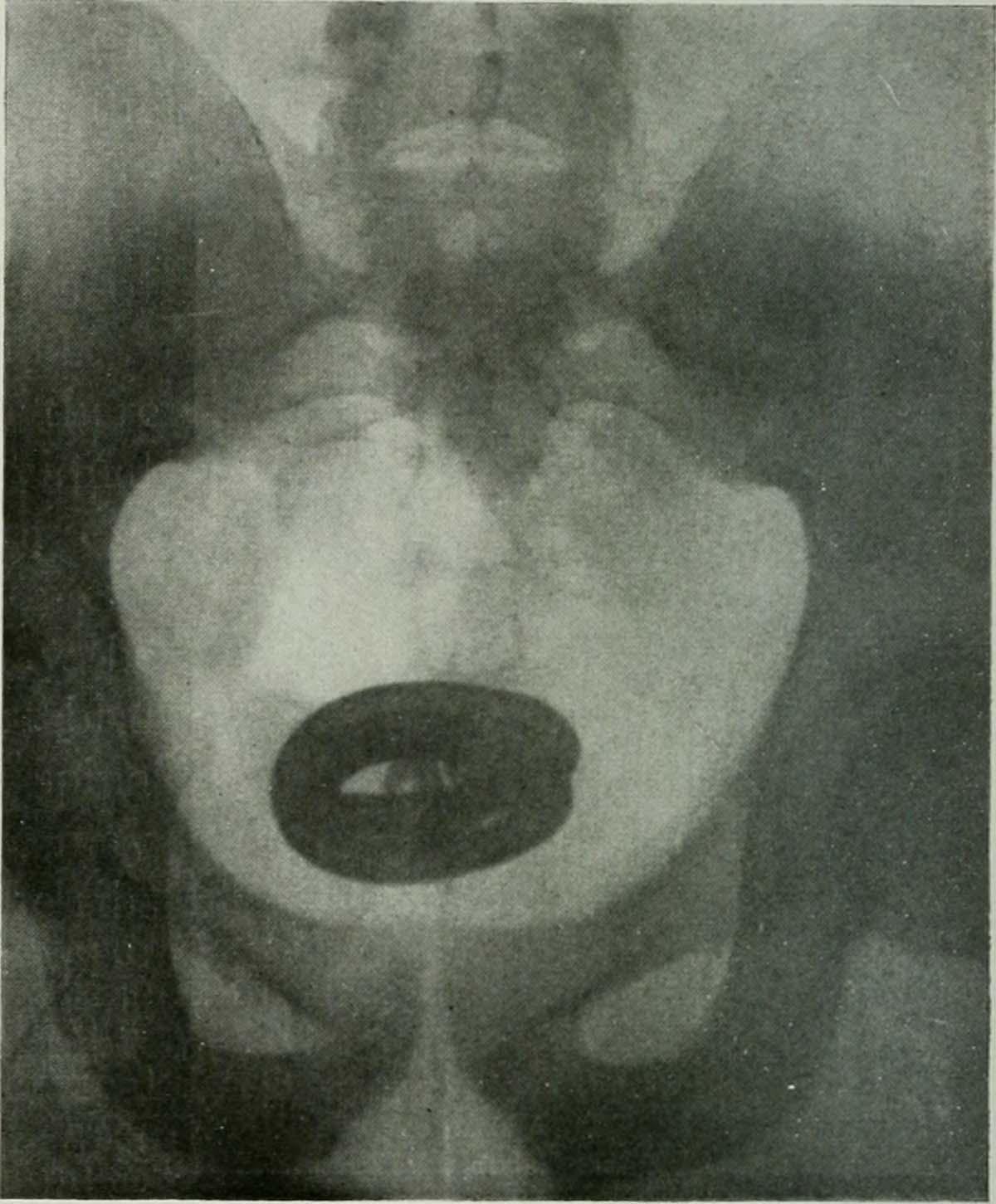
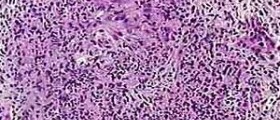
When it comes to pathophysiology of acute glomerulonephritis, the changes affecting the glomeruli are in the form of in situ formation of immune complexes. Associated inflammatory reaction may contribute to kidney enlargement. The affected kidneys might enlarge up to 50%. Histological characteristics include edema of the glomerular tufts and the presence of polymorphonucelocytes. A specific microscopic exams additionally reveal deposition of immunoglobulins and complement.
Medical experts are many times uncertain about the underlying causes of the formation of immune complexes. Only in case of poststreptococcal glomerulonephritis the recent Streptococcal infection of the throat triggers abnormal reaction of the immune system. It, after some time, evolves into glomerulonephritis.
The affected kidneys suffer specific structural changes which subsequently reflect on the very function of the kidneys.
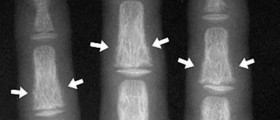
First of all there is clear proliferation of endothelial, mesangial and epithelial cells of the glomeruli. Furthermore, the inflamed tissues are infiltrated with neutrophyles and monocytes, both of which are types of white blood cells. There is also thickening of the glomerular basement membrane. In case microscopic evaluation reveals hyalinization, the damage to the kidneys is considered irreversible. All the aforementioned changes might occur focally, be diffuse or segmental and in rare cases are global.
Additionally, since the structure of the organ significantly changes, it is obvious that the affected kidneys will not function adequately. Namely, there will be functional changes such as hematuria, proteinuria and oligoanuria. The urine sediment will be rich in red blood cells and red blood cell casts. Insufficient elimination of sodium will result in water retention and accompanied hypertension and edema. All in all, damage to the kidneys affects these organs but also reflects on the entire body precipitating systemic health problems.
Signs of Acute Glomerulonephritis
It is possible that physical exam might not reveal any specific changes. However, most patients are confirmed with elevated blood pressure, there is a combination of edema and their urine output is significantly reduced.
Water retention leads to swelling of many parts of the body. Periorbital edema and/or pedal edema are two most common forms. As a matter of fact these edemas together with increased blood pressure affect around 75% of all patients suffering from acute glomerulonephritis.
More severe forms of edema affect internal organs such as the lungs. Excess of fluid inside the lungs is medically known as pulmonary edema. This is a medical emergency and highly lethal complication of glomerulonephritis. It is characterized by shortness of breath, grunting, gurgling and wheezing sounds while breathing, inability to speak in full sentences, excess sweating, cyanosis etc. Lack of oxygen might result in loss of consciousness. Auscultation of the lungs reveals crackles while the pressure in the jugular veins increases which contributes to their bulging.
Excess of fluid due to renal failure may also contribute to ascites (fluid build-up in the peritoneal cavity) or pleural effusion (fluid build-up in the pleura). Water retention in general can be easily confirmed by rapid weight gain.
Apart from the mentioned physical exam might reveal skin rash that resembles the one in patients suffering from Henoch-Schönlein purpura, or lupus nephritis.
The treatment for acute glomerulonephritis must be aggressive, efficient against inflammation and additionally comprise supportive care. Patients are hospitalized. The underlying cause of renal malfunction must be identified and treated as well. The cause of kidney inflammation determines the basis of the treatment. Complications such as edema, hypertension, oliguria etc. require specific drugs. Most of them are administered intravenously because this way they quickly achieve desirable concentrations in blood and fulfill their purpose. Corticosteroids act against inflammation, antibiotics fight off bacteria while antihypertensive bring the blood pressure under control and boost fluid excretion.
Bed rest and dietary changes (limitation of salt, fluid and potassium intake) are integral part of the treatment.
In rare instances, there is progression of the disease. The kidneys get affected by sclerosis and completely lose their function. These patients end up with renal failure. Those who recover might have abnormal urinanalysis for years even though the symptoms improve soon after the onset of treatment.
Fortunately the majority of patients fully recover and only in rarely one develops additional complications in the form of hypertensive retinopathy, hypertensive encephalopathy, rapidly progressive glomerulonephritis, chronic renal failure and nephrotic syndrome.















Your thoughts on this
Loading...