Acute polyarthritis is an inflammation of many joints and may develop due to different underlying causes. Because of that, this multiple joint inflammation many times leads to diagnostic difficulties.
In patients suffering from this type of arthritis, there are more than 5 joints affected at the same time. Acute polyarthritis is most commonly of autoimmune origin. It affects people of all ages and is equally distributed between genders.
In order to confirm the condition and identify its underlying causes, doctors should engage in careful clinical assessment and suitable investigations. In spite of having many tests and exams available to determine the actual cause of the condition, it may remain unknown.
What is Important for Proper Diagnosis?
Doctors can benefit from data regarding patient's age, sex, ethnic origin and occupation. Family history is also of great importance when diagnosing polyarthritis and identifying its underlying cause. For instance, children are in most cases affected by juvenile chronic arthritis. Furthermore, a family history of rheumatoid arthritis, seronegative arthropathies etc may drive a doctor to suspect the same condition.
While pain is a common complaint and is not efficient in diagnostic terms, speed of the onset may be very useful. In people suffering from gout the attack is abrupt while the onset of rheumatoid arthritis is more gradual. The time when pain occurs is also a valid data that may help in setting of definitive diagnosis.
Pattern of joint involvement can also help doctors to assume the type of arthritis a person is suffering from. Migratory arthritis is common for gonorrhea and rheumatic fever and may affect people suffering from systemic lupus erythematosus, sarcoidosis and Lyme disease. Furthermore, large weight-bearing joints are predominantly affected in osteoarthritis. This condition also affects facet joints of the spine in many cases. Younger individuals with axial involvement most commonly suffer from ankylosing spondylitis or inflammatory bowel disease associated arthropathy. Symmetry of the affected joints is one more clue that can drive a doctor to final conclusion. And finally, in patients with extra-articular symptoms setting of the diagnosis may be sometimes easier.
What Tests and Exams Does a Doctor Conduct?
Doctors routinely check patient's temperature and perform thorough physical examination. They pay special attention to nail changes, look at eyes for sigs of inflammation and palpate regional lymph nodes to check whether these are enlarged.
The skin is examined for signs of rash and vasculitis. Additionally, cardiac function examination, abdominal examination as well as examination of other systems are performed.
The affected joints are thoroughly examined and tested. The doctor investigates the skin around the affected joint and its mobility.
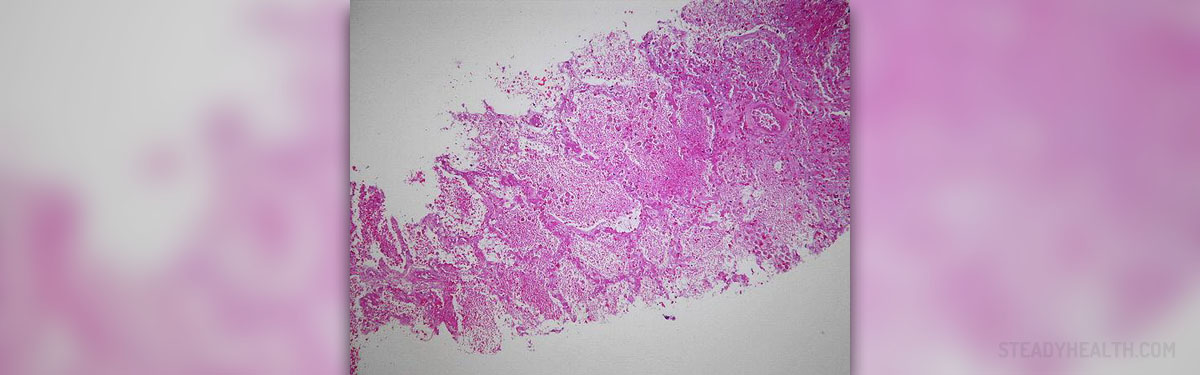
Diagnosing continues with different laboratory test and imaging studies and in some cases in order to set definitive diagnosis patients must undergo tissue biopsy.













-Symptoms,-Diagnosis,-Treatment_f_280x120.jpg)



Your thoughts on this
Loading...