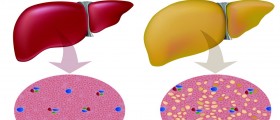
The term cirrhosis of the liver refers to the formation of scar tissue that can destroy the makeup of the liver. In the majority of cases, this condition occurs as a result of alcohol abuse. However, there are several other major causes of liver cirrhosis. This condition prevents the proper function of the organ, which can have negative effects on digestion and metabolism. As few as 30% of patients will survive the condition.
Causes
Excess alcohol consumption is a primary cause of the disease, accounting for about fifty percent of all cases of liver cirrhosis.
Other causes of the condition can be viral in nature. Hepatitis is one such cause. Hepatitis B and C are commonly seen to be causes of the condition. Autoimmune chronic active hepatitis is a rare condition that causes the immune system to attack the body, thus destroying liver cells.
Primary biliary cirrhosis is a disease whose cause is not entirely understood. The disease, mainly seen in females, causes the body to attack the liver.
Some chemicals and drugs can cause liver damage. However, it is relatively rare to see cirrhosis of the liver occurring as a result of contact with these substances. Some congenital disorders can lead to the build-up of toxins within the liver, the most common of which is hemochromatosis.
- A total of 1,071 patients with AD were enrolled. We collected detailed pre-specified information on the 3-month period prior to enrollment, and clinical and laboratory data at enrollment. Patients were then closely followed up for 3 months. Outcomes (liver transplantation and death) at 1 year were also recorded.
- Three groups of patients were identified. Pre-ACLF patients (n = 218) developed ACLF and had 3-month and 1-year mortality rates of 53.7% and 67.4%, respectively. Unstable decompensated cirrhosis (UDC) patients (n = 233) required ?1 readmission but did not develop ACLF and had mortality rates of 21.0% and 35.6%, respectively.
- Stable decompensated cirrhosis (SDC) patients (n = 620) were not readmitted, did not develop ACLF and had a 1-year mortality rate of only 9.5%.
- The 3 groups differed significantly regarding the grade and course of systemic inflammation (high-grade at enrollment with aggravation during follow-up in pre-ACLF; low-grade at enrollment with subsequent steady-course in UDC; and low-grade at enrollment with subsequent improvement in SDC) and the prevalence of surrogates of severe portal hypertension throughout the study (high in UDC vs. low in pre-ACLF and SDC).
Symptoms
The early stages of the condition might be asymptomatic, but as the disease progresses, one might begin to experience weakness, energy loss, tiredness, lack of appetite, nausea, and weight loss. The later stages will see the development of jaundice, nail changes, skin changes, fluid retention, spider veins, the tendency to bruise easily, and, in some cases, the development of male breasts.
Some symptoms of the very late stages of the disease include vomiting blood, and stomach ulcers. These symptoms indicate a need for immediate medical attention.
Treatment
Treatment will depend on the cause. If hepatitis is the cause, then the approach will revolve around combating that particular condition. The same applies to all the other medical conditions that cause liver cirrhosis.
If the cause lies in alcohol excess, you must cut down your intake of alcohol as soon as possible. Even small amounts can damage the liver after damage has occurred. It will also be necessary to make some positive lifestyle changes. If possible, lead as active life as you can. Tiredness may prevent this but try to persevere.
Look to maintain as healthy a diet as possible. Don’t add salt to your meals, and if necessary, employ the usage of vitamin and mineral supplements.
Treatment for cirrhosis of the liver will variously involve the use of diuretics, vitamin and mineral supplements, laxatives, or propranol. In severe or life-threatening cases, a liver transplant is the only option.
- www.nhs.uk/conditions/cirrhosis/
- medlineplus.gov/ency/article/000489.htm
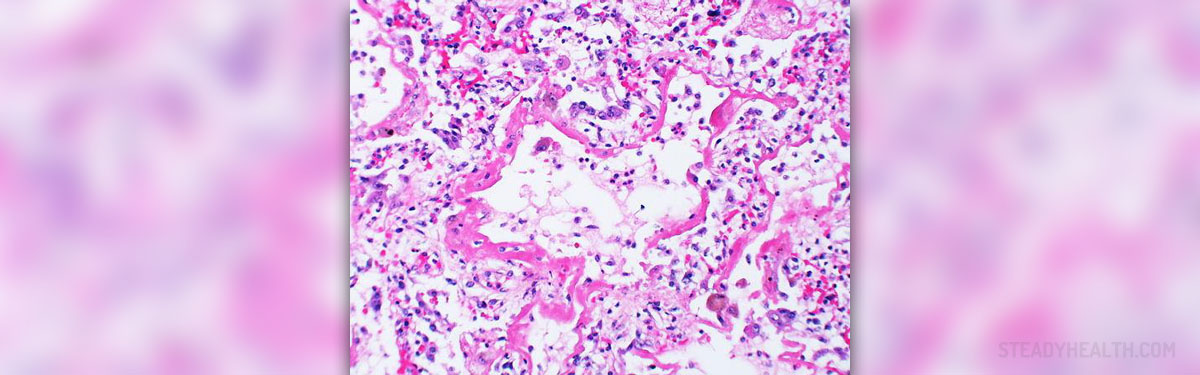
- Photo courtesy of Yale Rosen by Wikimedia Commons: commons.wikimedia.org/wiki/File:Acute_diffuse_alveolar_damage.jpg













Your thoughts on this
Loading...