Edema Causes
Edema is defined as excessive accumulation of fluid in the tissues and spaces between them. The formation of edema is basically related to three important factors: the quality of the blood vessel wall the value of the hydrostatic pressure the value of the osmotic pressure When the integrity of the blood vessel wall is damaged, its function of selective permeability is compromised and it becomes permeable to proteins that go from the blood into the tissue, carrying the water together with them and causing the occurrence of edema.The permeability of blood vessels is affected by various factors which include:prolonged hypoxia increased content of inflammation mediators neural regulation disorderpresence of toxins, especially poison gases nonvascular changes - lymph flow disordersdisturbances of entering the lymph in the blood increased lymph flow due to lower protein content in the blood (fluid passes from the blood into the tissues and hence into the blood vessels) - a dynamic lymphatic insufficiency. Lymph flow disorders can lead to specific clinical condition which is called elephantiasis.
Edema Types
They are classified according to etiology: cardiac edemakidney edemahepatic edema allergic edematoxic edemaCardiac EdemaReduced pumping blood from the left atrium as a result of various factors (coronary disease, valvular damage, atherosclerosis) leads to transmission of pressure through the small blood flow to the right side of the heart and hence the venous system, causing venous routes and cardiac insufficiency.
From there, the process of formation of edema has two directions: Venous route leads to increased venous pressure of the capillary network. Therefore, the hydrostatic pressure in the venous part of capillaries increases, causing returning fluid from the tissues into the circulation and edema. The second direction involves the arteries in which occurs the arterial hypovolemia that stimulates the renin angiotensin system. This further stimulates the secretion of aldosterone, causing the retention of water and salts in the kidneys. Later, there is an appearance of some phenomena that favor the formation of edema due to hypoxia: Increasing the permeability of blood vessels - hypoxia in the tissues due to routes in the blood vessels causes damage to blood vessels as they became permeable to proteins. Compromised synthetic liver function - hypoxia impairs synthetic liver function that is responsible for the occurrence of albumin - hypoproteinemia. Compromised renal excretory function - hypoxic damage to the kidneys causes increased permeability of epithelial ducts, so little protein that was left, go into the urine. Cardiac edema is static and localized firstly to the lowest parts of the body with the largest veins - the legs. Impression arises by pressing the swollen spot because the fluid is localized in the extracellular space. Hepatic Edema
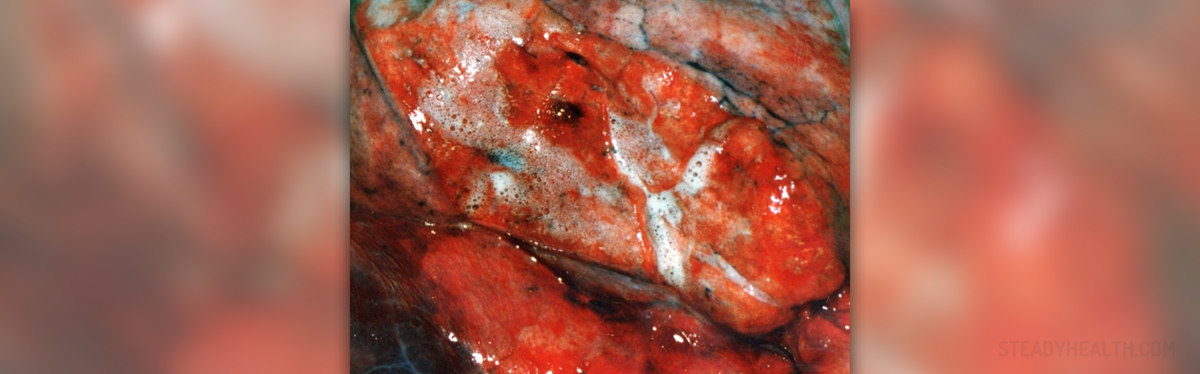
They are associated with liver cirrhosis. Liver cirrhosis is the replacing liver cells with connective cells. Binder, that dwelt in the liver, later contracts and deploys around the blood vessels, narrowing them and increasing the pressure in them. This pressure is transferred to the portals and portal vein blood flow, causing outpouring of fluid in the abdomen, and ascites formation.
Reducing the number of hepatocytes decreases synthetic ability of the liver and hypoproteinemia occurs, favoring the occurrence of edema.
Allergic Edema
Releasing mediators that increase permeability of blood vessels occur as a result of an allergic reaction. Toxic Edema
The endothelium of blood vessels is damaged and their permeability is increased due to action of chemicals (salts of heavy metals, arsenic, bile acids), effects of bacterial toxins (diphtheria toxin) and actions of animal toxins (spider, scorpion and snake bites), causing edema.

















Your thoughts on this
Loading...