The lacrimal system or the lacrimal apparatus of the eye comprises several components all of which participate in production of tears and their drainage. The system consists of the lacrimal gland, the lacrimal canaliculi and specific nerves. Tears are secreted by the lacrimal gland and after being distributed over the entire surface of the eye they are collected with the lacrimal canaliculi and carried by the nasolacrimal duct into the nasal cavity. The innervation of the lacrimal apparatus originates from the carotid plexus and some branches of the facial nerve.
Blocked Tear Duct
If tear ducts are blocked tears cannot be properly drained and they will flow down the cheeks. The affected individual will look as if he/she is crying. Now blockage of this type may be congenital or acquired. Many babies are actually born with underdeveloped tear-duct system which may easily lead to blockage, excess tearing and accompanying infection.
Blocked tear duct usually affects infants. It is estimated that one-third of all babies are suffering from this medical condition. It may resolve spontaneously within a year in up to 90% cases while the rest of the babies require specific treatment. It is essential to confirm the blockage as soon as possible and prevent potential infections.
Congenital nasolacrimal duct obstruction (dacryostenosis) is the leading cause of this type of obstruction. The duct is generally blocked by a tiny membrane. The membrane may rupture spontaneously or with the assistance of the parents (massage) and only if this is not achieved within certain period of time, babies are treated with more invasive treatments.
In adults blockage is acquired and associated with nasal polyps or cysts both of which may develop near the nasolacrimal duct, compress the nearby tissues interfering in the draining process. Similar scenario occurs in individuals suffering from tumors of the nasal cavity and those who have had an injury to the eye area which is severe enough to cut through the tear ducts.
In the majority of cases of congenital nasolacrimal duct obstruction symptoms and signs develop between the birth and the 12th week of age. It is also possible to confirm the condition once the infection occurs. Now, the clear sign of obstruction is excessive tearing, even when the child is not crying. Infection is located in the inner corner of the eye when pus might drain and cause crusts over the eyelids that generally develop over the night. Infection of the lacrimal gland leads to redness of the inner corner of the eye. The affected area is tender to touch. Palpatory exam reveals a bump or swelling in the inner corner of the eye.
Surgery for Tear Duct
Initially, parents are taught how to perform a massage of the blocked tear duct. The affected area should be massaged several types per day. Additional help is obtained from warm compresses which when applied onto the eye may promote drainage and ease discomfort. If the child develops infection, he/she is prescribed antibiotics in the form of eye drops and ointments. The drugs do not deal with the obstruction but only bring infection under control. The goal of the massage is to pop the membrane blocking the tear duct.
If massage fails to unblock the affected tear duct, the child suffers from repeated infections and excess tearing simply does not stop, the tear duct is treated surgically. The surgery is successful in 85-95% of all children who are up to 1 year old. The success rate is not that high if the child is older.
The first approach is surgical probing. The procedure is performed by a well-experienced ophthalmologist. The child leaves home immediately after the procedure unless the eye is affected by severe infection requiring hospitalization.
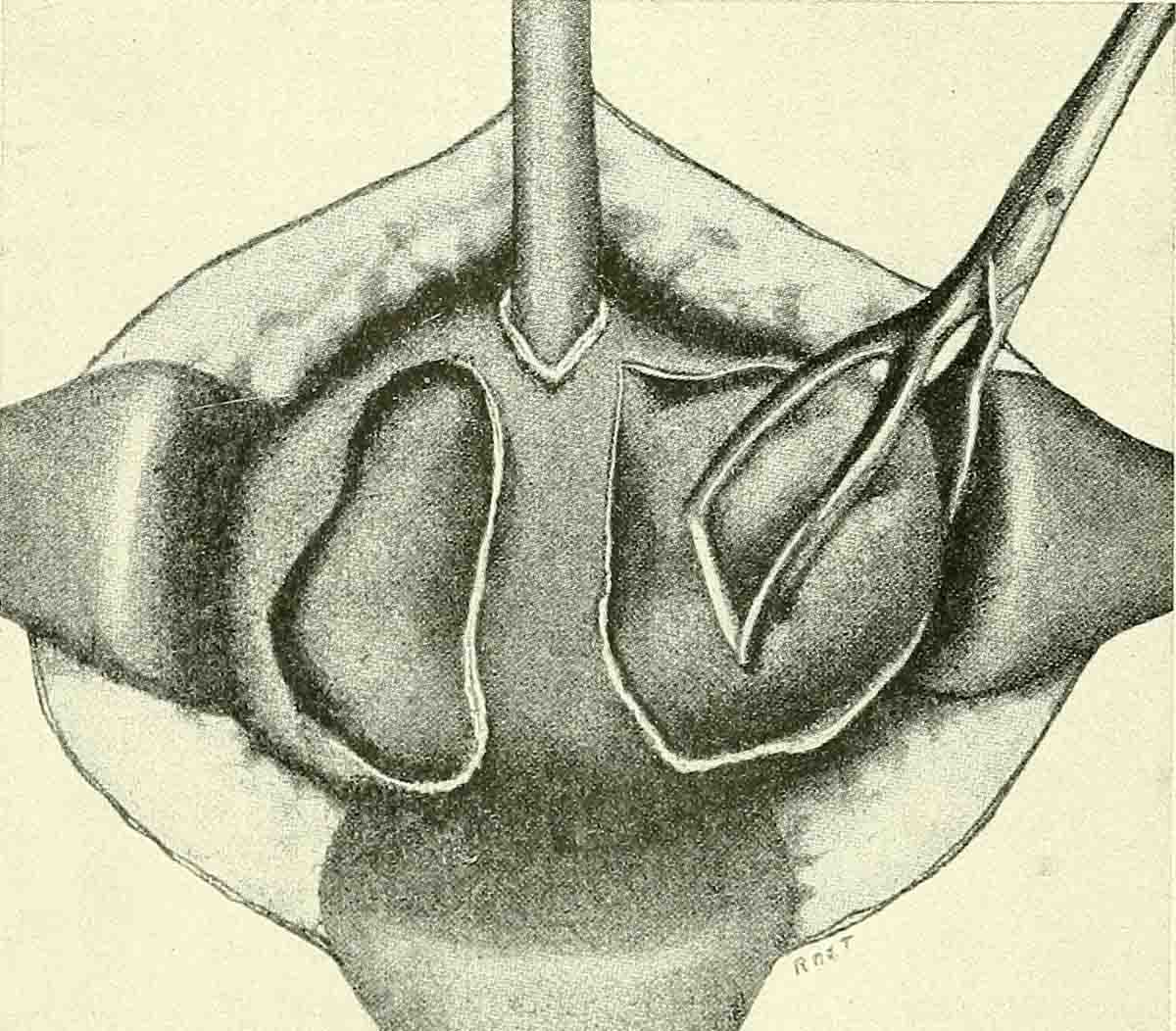
Prior to probing the doctor will examine the affected eye and rule out other conditions that might resemble tear duct obstruction. Once this is done, a thin and blunt metal wire is gently inserted into the tear duct and passed until it reaches the nasal cavity. The probe will rupture the membrane responsible for the obstruction. The procedure is generally nor painful although it might be unpleasant and cause slight discomfort. Surgical probing should be repeated if the closure reoccurs.
Failure of the probing requires further surgical treatment. The child undergoes a so called silicone tube intubation. The doctor uses a silicone tube and by inserting it into the tear duct keeps the passage wide open. The tube is left in the tear duct for approximately 6 month. Its role is to stretch the duct.
Balloon catheter dilation is one more surgical approach for blocked tear ducts. A balloon gets inserted through the tear duct and is then inflated with a sterile solution. The bulging of the balloon will stretch the tear duct and makes it wider. Once this is achieved, the solution is drained and balloon removed.
All in all, the last two procedures have similar success rates as probing. The results are evident after a week or so. Potential infection associated with the mentioned procedures is evaded with the assistance of antibiotic eye drops and ointments.















Your thoughts on this
Loading...