Fluid in Lungs
Fluid in lungs, medically known as pulmonary edema, is a life-threatening condition that features an accumulation of fluid in the lungs. This fluid interferes with the exchange of oxygen and carbon dioxide causing respiratory failure. Patients suffer from shortness of breath, and if left untreated, the lethal outcome is inevitable.
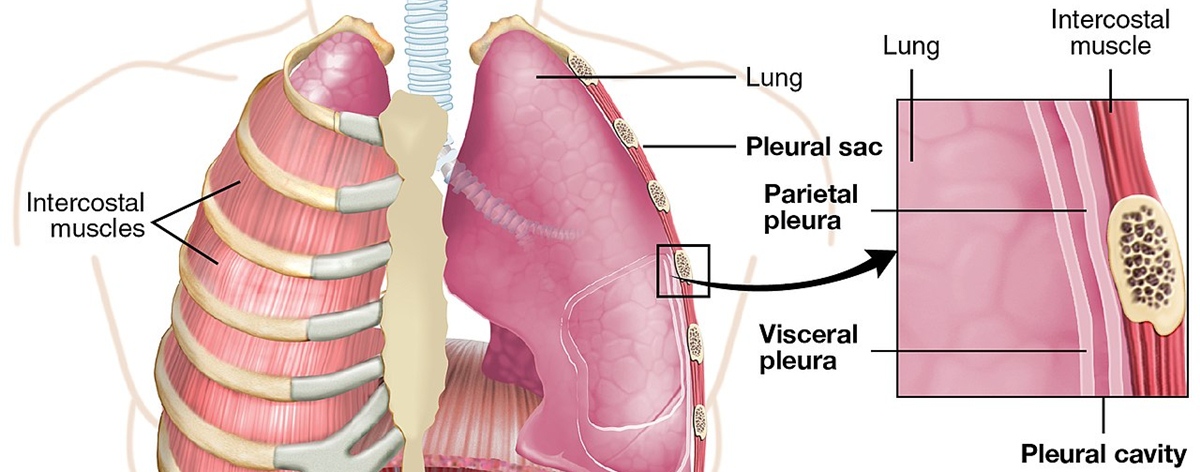
By auscultating the lungs of patients who are suffering from pulmonary edema, a doctor can hear a bubbling sound that accompanies the breathing pattern. This sound is specific for the accumulation of fluid in lung tissue or inside the pleura.
There is a difference between the previous two. Namely, pleural effusion is the collection of fluid that accumulates inside the pleura, while in pulmonary edema, fluid accumulates inside the alveoli. This is why simple auscultation can only confirm the presence of the fluid but cannot differentiate where the fluid exactly is.
Symptoms of Fluid in Lungs
The symptoms of this medical condition may vary especially in intensity. The most significant thing is to recognize them at the start and to administer appropriate medications as soon as possible.
The first thing a doctor will notice is rapid breathing and shortness of breath. It may sometimes look as if the patients are struggling for breath. Patients are weak and exhausted. Their skin is pale and wet because they sweat a lot. An additional symptom is cough and the mucous may resemble foam with traces of blood.
Anxiety and restlessness are usual consequences since patients are frightened. The situation only gets worse if the patients are trying to lie down. The symptoms may improve in sitting or standing positions. The symptoms may be so severe that patients simply cannot talk. And finally, auscultation of the lungs points to bubbling noise, which accompanies breathing.
Causes of Fluid in Lungs
The intensity of the symptoms depends on how much fluid has accumulated inside the lungs. The alveoli are filled with mucus and fluid, which enters from the smallest blood vessels called capillaries.
Pulmonary edema may be a consequence of a variety of medical conditions. It most commonly occurs in heart failure. Even renal failure results in fluid in the lungs. Apart from that, it can also accompany different lung infections such as bronchitis, pneumonia, or tuberculosis. Another cause of fluid in the lungs is allergies.
- Pulmonary edema is the disequilibrium between formation and reflux of lung tissue fluid leading to the absorption of massive tissue fluid by lung lymph and vein failure. The fluid transudes into and accumulates in the interstitium of lungs and finally alveolars from lung capillary, leading to severe disorder of pulmonary ventilation and gas exchange. In COVID-19 patients, pulmonary edema is diagnosed by lung ultrasound and a computerized tomography (CT) scan.
- SARS-CoV-2 invasion leads to alveolar and vascular epithelial cells damage impelling the formation of minimal thrombus, increasing pulmonary venous pressure and vascular permeability and leading to massive loss of tissue fluid. Besides those direct causes of COVID-19 pulmonary edema, there are other factors that can be described as abnormal humoral metabolism which can influence the AFC and PFC, resulting the manifestation of pulmonary edema.
- Immune-modulatory agents for COVID-19 include tocilizumab, human immunoglobulin and the convalescent plasma. IL6 monoclonal antibody or tocilizumab was thought to work by interrupting inflammatory storm after the infection, but the latest clinical study published in NEJM showed that Tocilizumab was not effective in preventing intubation or death in mild hospitalized COVID-19 patients.
Inhalation of smoke or other caustic chemicals may lead to pulmonary edema. It can additionally be a side effect of certain medications or narcotics.
Furthermore, fluid in the lungs occurs in drowning, hypoalbuminemia, and some autoimmune disease. And this medical condition can also accompany lymphatic insufficiency.
- www.ncbi.nlm.nih.gov/books/NBK557611/
- medlineplus.gov/ency/article/000140.htm
- Photo courtesy of OpenStax College by Wikimedia Commons: commons.wikimedia.org/wiki/File:2313_The_Lung_Pleurea.jpg
















Your thoughts on this
Loading...