The first indication that a patient suffering from Dupuytren’s disease needs surgery is when the deformity interferes with normal physical function. Otherwise, the condition is likely to be treated differently. If contracture is present it can indicate that further examination is in order.
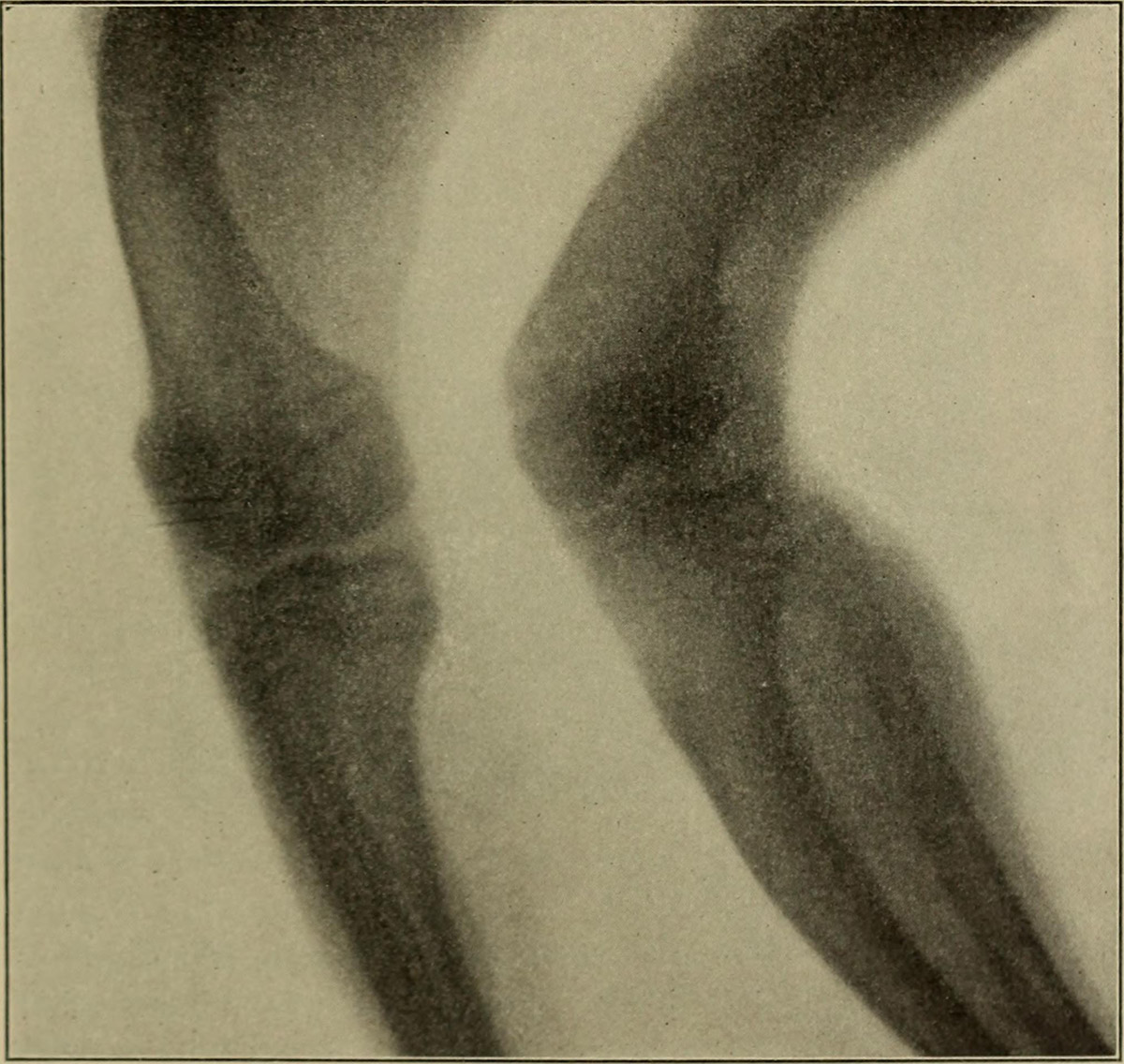
By some sources, any physical observation revealing a flexion contracture of 10-15 degrees is reason enough for further examination. A flexion contracture exceeding 15 degrees (or 30 when it comes to the MCP contracture) is enough to recommend a surgery.
The procedure is aimed at correcting the deformity and restoring functionality. Complications are usually minimal, if any. MCP joint correction surgery is usually more successful than the PIP version. MCP joint contractures in general tend to respond very well to surgery, even after a prolonged condition. This is rarely the case with PIP joint contractures.
Along with the usual risks involved with any surgery (bleeding, infection, anesthetic complications etc.) there is a number of possible consequences specific to Dupuytren’s disease treatment. The main concern is nerve damage, which can occur for many different reasons. Necrosis of the tissue is also an issue. Delayed healing may result from vascular complications or direct injuries. Another one is stiffness of the joints.
Although the success rates are good, the surgery often proves to be only a temporary solution. Studies have shown that recurrences happen as often as 60 percent of the time. The most comprehensive of these studies concluded that the recurrence happens around somewhere between 50 and 60 percent of the time. These results are linked to PIP joint release only. The MCP procedure shows much more favorable results. Remarks were made that studies associated with this condition rarely differentiate these two procedures, thus diminishing their conclusiveness.
Surgical procedures available to treat this ailment include fasciectomy, limited fasciectomy, dermofasciectomy, segmental aponeurectomy, percutaneous needle fasciectomy and extension device implementation.
Recovery period involves some preoperative planning. Therapy is almost fully directed at restoring the function of the hand. A mildly compressive dressing will be applied after the procedure, but the joints will be exposed enough so that the flexion is unobstructed.
Once the dressing is removed, wound care becomes more important, followed by active and passive flexion.
The postoperative program is also aimed at controlling the edema. Once the edema subsides, flexion will gradually become easier. Full closure of the wound should also become possible at this time. Active therapy is very important. It should last for at least six to eight weeks.
















Your thoughts on this
Loading...