The spleen is an internal organ located in the abdomen, with a few functions all of which are associated with red blood cells and the immune system. Namely, the organ removes old erythrocytes (red blood cells), participates in the metabolism of hemoglobin and also serves as a reservoir holding some amount of blood in case severe hemorrhage takes place. The spleen also produces antibodies and at the same time eliminates antibody-coated bacteria together with antibody-coated blood cells from systemic circulation. And finally, the recent findings have confirmed that approximately a half of all body's monocytes are located in the organ. These white blood cells are of major importance for tissue injury.
Splenectomy for Removal of the Spleen
Surgical removal of the spleen is medically known as splenectomy. The spleen is the organ we can live without and there are specific indication when it is removed.
The spleen is one huge reservoir of blood and a powerful filter capable of eliminating old blood cells as well as microorganisms from the body. What is more, the organ is a site for the development of new erythrocytes from their precursors, especially when the process of hematopoesis cannot take place in the primary organ in charge of this function, the bone marrow.
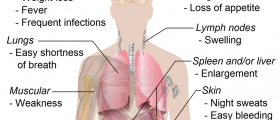
Even though the spleen may enlarge in certain conditions such as mononucleosis, malaria and certain cancers (predominantly leukemias and lymphomas), its removal is not an option for all patients.
First of all, the spleen is surgically removed if it becomes very large and consequently starts to destroy healthy platelets or red blood cell, precipitating a drop in their blood counts.
Furthermore, if the organ is affected by leukemic cells or lymphoma and there is no further dissemination of the diseases, the spleen might be removed.
Additionally, splenectomy is performed in case of wandering spleen, destruction of platelets by the organ due to an underlying auto-immune process and when there is severe bleeding from the organ that jeopardizes person's life.
The organ is also removed when patients suffering from congenital erythropoietic porphyria (CEP) develop severe form of hemolytic anemia. Splenectomy is a treatment option for congenital pyruvate kinase (PK) deficiency too.
And finally, if the organ is affected by gastric cancer or the doctors need to use the splenic artery when performing kidney revascularization, they first perform splenectomy.
The very procedure is not complex. Laparoscopic approach is sufficient enough in case the spleen is not too large and when the surgery is classified as elective. On the other hand, open surgery is the only option when the organ is severely enlarged and there is a risk of spontaneous rupture. Open surgery allows surgeons to have full insight in the abdominal cavity and act promptly even when during the removal the organ bursts.
Both of these surgeries are invasive and require general anesthesia. Patients who are scheduled to have splenectomy are supposed to be vaccinated against Pneumococcus, Hemophilus influenzae and Meningococcus. The vaccination will significantly reduce the risk of postoperative infection known as post-splenectomy infection which is associated with rapid and sometimes lethal type of sepsis.
The organ removal includes separation of the spleen from its arteries as well as the ligaments that hold it in its place. Some people have one or two additional spleens which are referred to as accessory spleens. They are removed together with the major organ. The abdomen is closed and there is a drain left inside the peritoneal cavity which will allow excess of fluid to be eliminated. The drain is removed after a couple of days. In the majority of cases the resected spleen is sent for pathohistological examination.
Splenectomy Procedure Risks
As it has already been mentioned practically all patients who undergo splenectomy are at risk of developing postoperative sepsis. Still, the chances for this complication to occur can be reduced with the assistance of several vaccines including the pneumococcal conjugate vaccine, Hib vaccine and the meningococcal vaccine. The bacteria these vaccines are efficient against generally cause mild issues such as sore throat but if the spleen is removed they may be very harmful to the body even leading to death.
Splenectomy is usually accompanied by an increase in the number of white blood cells and may be a cause of high platelet count. Excess of platelets is connected with clot formation and associated health problems such as pulmonary embolism. So, when the number of platelets becomes too high doctors should introduce certain anticoagulant agents.
Some studies have pointed that operated patients are at higher risk of developing diabetes although this hypothesis needs more evidence. Bleeding, infections and injuries to the nearby organs are several more potential side effects of splenectomy.
And finally, one of the complications that cannot be corrected is chronic neutrophilia.
Given all the mentioned it is clear that even though we can live without the spleen its removal is not a benign procedure and may cause sometimes serious complications. Nevertheless, when performed by well experienced surgeons and with proper preparation and aftercare most adverse effects are evaded and patients continue with their lives without any further problems.











Your thoughts on this
Loading...