Intestinal Pain after Eating
Intestinal pain is denoted by an uncomfortable or painful sensation in the abdomen and is primarily linked with other problems with the digestive system. The frequency, strength, and type of pain will vary due to other circumstances affecting the intestine or the digestion system.
Sometimes, the intestinal pain will be a sharp, stabbing sensation that fades quickly but returns often, occasionally causing muscle cramping. Other times the pain may be fairly strong but dull and spread out and may last for hours at a time. Pain may be so intense as to induce nausea and vomiting in some people.
Causes and Symptoms
There are many different reasons that different people will experience discomfort or pain in the abdomen after eating. Certain disorders of the digestive system can contribute to this. Other factors include the type of foods being consumed; spicy or fatty foods can cause indigestion or infection of the stomach lining or the intestinaltract
IBS, or irritable bowel syndrome, is a condition that affects the lower intestinal tract, typically caused by an infection, abnormal muscle contractions, or overly sensitive nerves reacting to outside stimuli. IBS results in cases of both diarrhea and constipation, naturally causing major discomfort.
Occasionally, an obstruction in the bowels is the cause of intestinal pain. The digested matter is blocked from exiting the body and builds up in the large intestine and colon, causing the muscles around the intestine to tense painfully. This can occur because of a bacterial infection, incorrect bowel function, or even food poisoning.
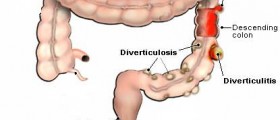
An inflammation in the wall of the intestine called diverticulitis can cause pain when pressure is exerted on the intestine due to the working of the digestive system, usually in the lower left abdominal area. Typical symptoms of diverticulitis include constipation, diarrhea, and fever.
Consuming dairy and dairy by-products while being lactose intolerant can lead to intestinal pain as the digestive system has trouble dealing with the lactose sugar present in those products. This typically manifests as abdominal discomfort, cramps, and bloating.
- The data analyzed originated from the Internet survey component of the population-based Rome Foundation Global Epidemiology Study, completed in 26 countries (n = 54,127). Adult subjects were asked whether they had abdominal pain and how often this was meal-related. Respondents were categorized into "no," "occasional," and "frequent" meal-related abdominal pain groups based on 0%, 10-40%, and ?50% of the pain episodes being meal-related, respectively. DGBI diagnoses, frequency of other GI symptoms, psychological distress, non-GI somatic symptoms, quality of life, and healthcare utilization were compared between groups.
- Mixed linear and ordinal regression was used to assess independent associations between psychological distress, non-GI somatic symptoms, quality of life, other GI symptoms, and meal-related abdominal pain.
- Overall, 51.9% of the respondents reported abdominal pain in the last 3 months, and 11.0% belonged to the group with frequent meal-related abdominal pain, which included more females and younger subjects. DGBI diagnoses were more common in subjects with frequent meal-related abdominal pain, and the frequency of several GI symptoms was associated with having more frequent meal-related abdominal pain.
- Having meal-related abdominal pain more frequently was also associated with more severe psychological distress, non-GI somatic symptoms, and a poorer quality of life. The group with frequent meal-related abdominal pain also more often consulted a doctor for bowel problems compared to the other groups of meal-related abdominal pain.
Diagnosis and Treatment
Diagnosis is typically difficult due to the number of factors that can cause intestinal pain and the similarity of these factors to each other. The doctor will first test to discover the characteristics of the pain by examining the abdomen directly and subsequently performing radiological or endoscopic tests if the diagnosis is still too vague. Medications are prescribed for the specific causes, and general dietary advice is given.
Generally, one can preclude intestinal pain by including high-fiber foods in meals and avoiding spicy, fatty, or sugary foods. Caffeinated or carbonated drinks may also contribute to abdominal discomfort. Drinking six to eight glasses of water is recommended by doctors as everyday habit, and it can also help in this case.
- medlineplus.gov/ency/article/000287.htm
- www.nhs.uk/live-well/eat-well/should-you-cut-out-bread-to-stop-bloating/
- Photo courtesy of Mikael Häggström by Wikimedia Commons: commons.wikimedia.org/wiki/File:Intestine_-_sized.png














Your thoughts on this
Loading...