Hemophilia Diagnosis and Treatment History
Hemophilia was first detected by the Jewish people, who created circumcision laws that imply the discovery of the condition as well as the fact it is passed on by the mother. The earliest account of hemophilia was recorded by Dr. John Conrad Otto, in 1803, who called it a 'genetic hemorrhagic disposition', and noted its hereditary nature and commonness in women.
The actual name 'hemophilia' was first recorded at the University of Zurich in 1828. Harvard doctors Patek and Taylor discovered the anti-hemophilic globulin in 1937, and a Buenos Aires doctor, Pavlosky, is credited with discovering hemophilia A and hemophilia B as triggers to more than one form of hemophilia.
Hemophilia was known as the royal disease due to Queen Victoria being a carrier of it, and passing the gene to many nobles such as Alexei, son of the Russian Tsar Nikolai.
During the 1900s, blood transfusion became a possibility, after a sufficient amount of blood was lost, but blood storage was not possible at that time. The usual life expectancy of hemophiliacs at the time was 13 years. Plasma was discovered in the 1950s, but it did not contain enough of the needed factor. This was remedied in 1965 with the advent of ’’Cryo’’, a Cryoprecipitate that settled in the bottom of a plasma bag and was consequently frozen and infused.
In the ’70s Factor concentrates became available, but caused the infection of more than 80% of the people with hemophilia in the U.S with HIV in the ’80s. Viral-inactivated factor products become available in 1985, and the first non-plasma-derived factor becomes available in 1992, by using recombinant DNA technology. Finally, in 1995, ’’Prophy’’ becomes the U.S. standard way of treatment. It works by taking factors regularly to prevent bleeding, instead of waiting for the bleeding to occur.
- The earliest description in ancient history dates from the second century AD in the Babylonian Talmud about a woman who had lost her first two sons from circumcision. The earliest description in modern history was documented by the American physician Dr. John Conrad Otto. Dr. Conrad described an inheritable bleeding disorder in several families where only males born from unaffected mothers were affected. He then called them the “bleeders.”
- Hemophilia, as a word, was first documented by Johann Lukas Schönlein in his dissertation at the University of Zurich, Switzerland. Dr. Nasse was the first to publish the genetic description of hemophilia in Nasse’s Law: which states that hemophilia is transmitted entirely by unaffected females to their sons.
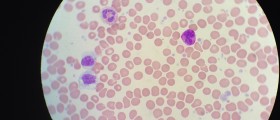
- Hemophilia is usually an inherited condition and is caused by the deficiency of clotting factors in the blood. It is almost always due to a defect or mutation in the gene for the clotting factor. Research has identified over 1000 mutations in the genes encoding factor VIII and IX, and around 30% are due to spontaneous mutation.
- Hemophilia is equally distributed among all ethnic groups worldwide. The estimated frequency of hemophilia is around 1 in 10000 live births, and the number of people worldwide living with hemophilia is about 400000. Hemophilia A is more prevalent (80% to 85% of the total hemophilia population) than hemophilia B. It presents in 1 in 5000 live male births, whereas hemophilia B presents in 1 in 30000 live male births.
- Hemophilia usually presents as bleeding after minor trauma or as a spontaneous bleed. Bleeding symptoms often correlate with the degree of residual factor level, which is useful to classify hemophilia severity further. Patients with greater than 5% to 40% of factor activity of normal (mild hemophilia) often present with bleeding only after significant trauma or surgery. Spontaneous bleeding is uncommon in mild hemophilia.
- In cases of severe hemophilia, patients often present with internal bleeding, potentially impacting multiple organs. Joints can become painful, swollen, inflamed, warm, and have a restricted range of motion due to bleeding. The most commonly affected joints are knees, elbows, ankles, shoulders, wrist, and hips. Spontaneous joint bleed incidence typically increases with age reaching up to 60% by 65 years of age.
Causes and Treatment of Hemophilia
Hemophilia is caused by a genetic deficiency that significantly lowers the blood plasma coagulation factor that is required for the blood to clot normally and is usually inherited from the mother. A hemophiliac does not bleed more than the average person but bleeds for a longer time. This causes a person suffering from hemophilia to lose lots of blood from even a minor injury, with bleeding that can last for weeks.
Internal bleeding and brain injuries can all prove fatal to hemophiliacs and can cause debilitation and complications such as hemorrhage, hemarthrosis, menorrhagia, and gastrointestinal bleeding. One in every 10.000 male and 1 in 20.000 female people are born hemophiliac. The condition can also be acquired during a person’s lifetime.
Hemophilia A is caused by the absence of the functional clotting Factor VIII in 90% of hemophilia cases. Hemophilia B is the result of the lack of Factor IX. Hemophilia C is autosomal, not X-linked, and is rare.
Frequent transfusions carry the risk of exposing the hemophiliac to viruses such as HIV and hepatitis. Any families with a medical history of hemophilia are advised to receive genetic counseling, and prenatal DNA testing can help detect the deficiency in time.
While there is no cure for hemophilia, it can be controlled with blood infusions and factor isolation within the blood serum. An anti-hemophilic, genetically engineered factor called Xyntha is used for the treatment, and though it is expensive, it is very effective. There is also the option of Prophylaxis, a procedure that involves the infusion of the deficient clotting factor periodically. Joint strengthening and muscle flexibility exercises can also help significantly.
















Your thoughts on this
Loading...