
What is Plasmapheresis?
Plasmapheresis is one of many treatment modalities. It actually includes selective removal of specific components from the plasma, the ones that are considered to be the culprits of the current disease. Once treated the remnant blood is then combined with replacement plasma and returned to the patient.
This is a type of extracorporeal therapy since plasma is manipulated with once it has been removed from the body. Plasmapheresis is indicated in many medical condition, predominantly autoimmune diseases.
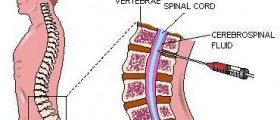
The very procedure is not complex although specific steps must be followed. The blood is taken through a needle or previously implanted catheter. Once the blood is drawn plasma is separated from other blood components with the assistance of a cell separator. The separation is achieved with discontinuous flow centrifugation, continuous flow centrifugation or plasma filtration. When discontinuous flow is engaged there is a need for only one catheter line. During this procedure approximately 300 mL of blood is removed. Continuous flow centrifugation is a bit different and requires two venous lines. The volume of the removed plasma is lesser compared to continuous flow centrifugation. And finally, in case of plasma filtration there are also two venous lines, the removed plasma undergoes filtration similar to those in hemodialysis and only 100mL of blood is removed in one session.
Each of the mentioned approaches has its own advantages and shortcomings. All in all, the plasma that has been removed is treated in a specific way and then returned to the patient's body. In rare instances doctors discard the removed plasma and patients receive certain replacement fluids. The procedure also requires anticoagulants which prevent blood clot formation and associated complications.
When it comes to more specific details regarding plasmapheresis, this procedure is basically performed on an outpatients basis. It can be rather uncomfortable but is never painful. furthermore, the number of sessions depends on the underlying condition as well as the patient's general condition. In the majority of patients plasmapheresis is done 6-10 times over the period of 2-10 weeks. Even though one session per week is usually sufficient enough, patients may sometimes have two.
Plasmapheresis is highly efficient treatment modality. Still, similarly to other treatments it carries certain risks and is associated with several side effects. Catheter insertion might result in bleeding. Left for a long period of time the catheter might also be a cause of local infections.
Furthermore, once the blood is removed from the body it succumbs its natural tendency to clot. To prevent blood clotting doctors use citrate together with the blood. Citrate binds to calcium this way preventing initiation of blood clotting process. However, this might cause negative effects to the body. Namely, once bound calcium cannot be used properly. The level of free calcium may significantly drop and precipitate symptoms and signs of hypocalcaemia. The hallmarks of the condition are the Chvostek's sign or Trousseau's sign. Fortunately, since today this complication is to be expected it can be successfully prevented if patients are administered calcium intravenously during the very procedure. What is more, patients might be prescribed calcium supplements that are taken orally.
And finally, there are a few more side effects of plasmapheresis including a drop in blood pressure, transfusion reactions, transfusion transmitted diseases, suppression of the patient's immune system and bleeding or hematoma at the site of the needle insertion.
Plasmapheresis and Autoimmune Diseases
Autoimmune disease are a specific group of illnesses all of which are characterized by the attack of the body i.e. its immune system which stops recognizing its own components. Namely, certain cells and tissues become the target of the components of the immune system because their receptors or proteins they contain may resemble foreign particles. This abnormal behavior of the immune system leads to detrimental effects and sometimes even permanent damage of the affected structures.
Plasmapheresis is indicated in various autoimmune disease. Still, it is never the first treatment option. Initially doctors try with different medications, most commonly corticosteroids but when patients fail to respond to the initial treatment they require more aggressive approach such as immunosupressants and similar drugs which might have serious side effects. One of the problems associated with immunosupression is that most patients receive high doses of these specialized drugs and they usually need to be taken for the rest of the patient's life.
One of the characteristics of certain autoimmune disease if not all of them is production of autoantibodies, the ones that destroy the cells of the body which are not recognized as a part of the body, but instead perceived as foreign particles. Plasmapheresis efficiently eliminated these autoantibodies from the bloodstream. By doing so, the damage to the target organs significantly reduces.
Currency plasmapheresis is used in patients suffering from myasthenia gravis, Guillain-Barré syndrome and is also very potent against chronic demyelinating polyneuropathy. However, not all autoimmune disease are treated with this treatment approach. The efficacy of plasmapheresis against, for example, multiple sclerosis or polyomyositis is yet to be established.











_f_280x120.jpg)

Your thoughts on this
Loading...