Supraventricular Tachycardia - Overview
Supraventricular tachycardia, also known as paroxysmal supraventricular tachycardia, refers to any tachycardia rhythm that originates from above the ventricular tissue. Fast heart rates caused by supraventricular tachycardia may be rather serious. There are two types of supraventricular tachycardia, atrioventricular nodal reentrant tachycardia- AVNRT and atrioventricular reciprocating tachycardia - AVRT which also includes Wolff-Parkinsons-White syndrome.
During the episode of supraventricular tachycardia, there is an evident abnormality in the functioning of the heart's electrical system. This results in a rapid heartbeat. Patients may experience up to 100 beats per minute and in severe cases, the heart rate can even reach 300 beats per minute. The treatment must be urgent and the goal is to normalize the heart rate to the normal value of 60 to 100 beats per minute.
The problem related to supraventricular tachycardia is that the episode can start and end quickly and the patients may not have any symptoms at all. Once the condition becomes serious and the attacks last longer or happen often the symptoms of tachycardia fully develop.
Supraventricular Tachycardia Causes and Symptoms
The actual cause of supraventricular tachycardia is in majority of cases associated with faulty electrical connections in the heart. It may also occur in people who take high levels of the heart medication digoxin or theophylline, a medication used in some lung conditions. Furthermore, a type of supraventricular tachycardia called Wolff-Parkinson-White syndrome may run in families. And finally, this condition can develop as a consequence of certain illnesses such as COPD and pneumonia.
Even though some patients may be asymptomatic the symptoms of supraventricular tachycardia usually include palpitations (feeling of a rapid heartbeat), pounding pulse, and feeling of dizziness and lightheadedness. Syncope, shortness of breath, chest pain, and sweating are possible as well.
Supraventricular Tachycardia Diagnosis
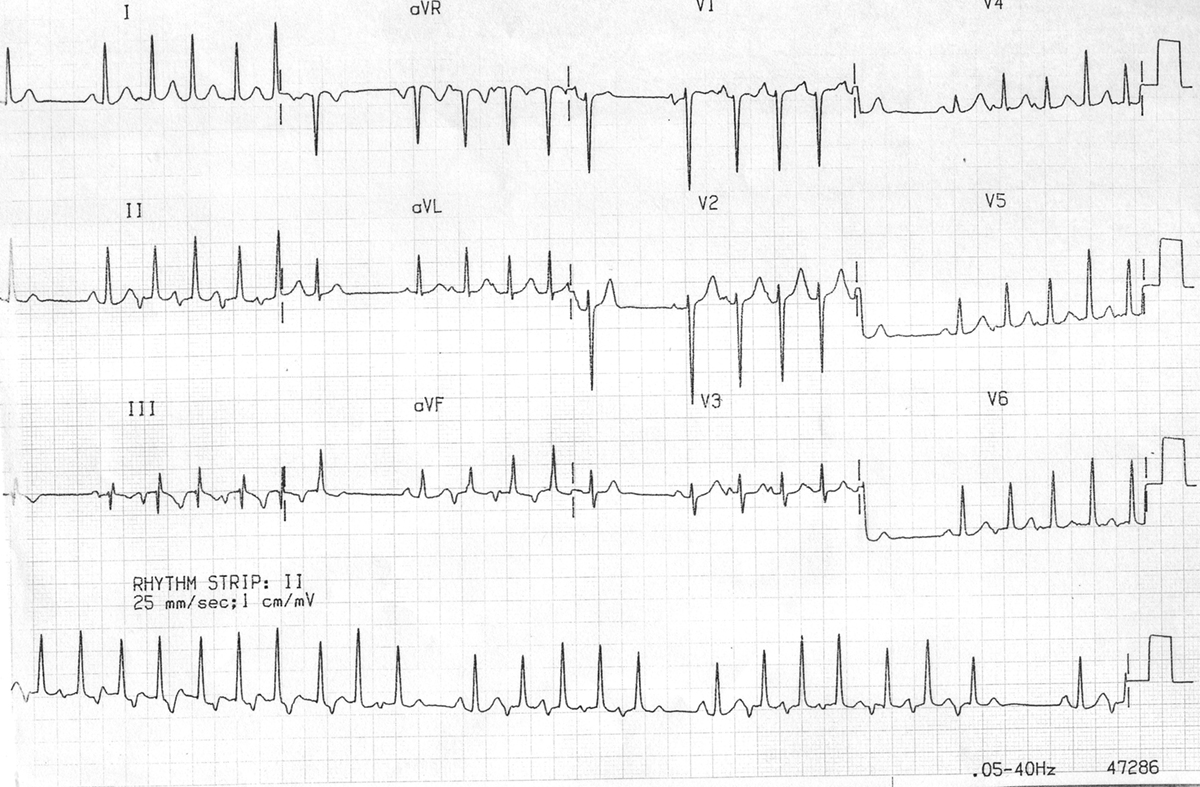
Diagnosis of supraventricular tachycardia is set after thorough questioning of the patient, physical exam, and the most significant test which confirms the presence of rapid heart rate and its characteristics called EKG (electrocardiogram). The patients additionally undergo an electrophysiology study.
Medicamentous and Surgical Treatment for Supraventricular Tachycardia
Supraventricular tachycardia can be initially treated with vagal maneuvers including gagging, holding one's breath or bearing down, etc. These maneuvers actually stimulate the vagus nerve and slow the heart's action. If these maneuvers do not work patients are given fast-acting medications such as adenosine or verapamil. And finally, if even these medications cannot slow down rapid heart rate the patient undergoes electrical cardioversion. This is a technique in which the application of an electrical current is included to reset the heart rhythm.
People who have frequent attacks are prescribed certain medications which are supposed to be taken on a regular basis. These medications can successfully prevent the reoccurrence of the attacks. Still many of these drugs have many side effects.
Surgical treatment for supraventricular tachycardia includes a procedure called catheter ablation. The goal of the procedure is to block abnormal electrical impulses. However, the procedure is very risky and may cause bleeding, infections, and even injury to the heart. This is why open heart surgery for supraventricular tachycardia is performed in rather rare cases.
- Between 2002 and 2013, 80 consecutive patients with CHD, mean age of 39 years, underwent intraoperative ablation with monopolar irrigated radiofrequency during cardiac surgery procedures.
- Significant clinical predictors of arrhythmia recurrence were determined by univariate analysis. We performed 47 right-sided Maze procedures, and 33 Cox-Maze III procedures. In 75 survivors, the ablation was effective immediately.
- Over an average follow-up period of 72 months (12-155 months), arrhythmias recurred in nine (20%) patients after right-sided Maze, and in six (19%) patients after Cox-Maze III. Eleven patients were controlled with medical therapy, three underwent catheter ablation of the arrhythmia, and one required a permanent pacemaker. Preoperative arrhythmia length ?3 years (P ? 0.001), tetralogy of Fallot (P ? 0.006), and preoperative atrial fibrillation (P ? 0.016) were associated with recurrence arrhythmia.
- Conversely, NYHA class

















Your thoughts on this
Loading...