
Pars planitis is only one type of uveitis, to be more precise it is the inflammation of the narrow portion of the cilliary body called the pars plana. The eye comprises three layers and the uvea or the uveal layer of the eye is the middle, pigmented, vascular layer made of the iris, cilliary body and choroid. Inflammation of the pars plana affects only the portion of the cilliary body and may be unilateral or bilateral.
Pars Planitis is a Form of Uveitis
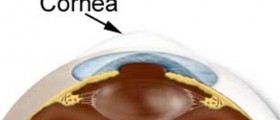
As it has already been mentioned pars planitis represents inflammation of the middle layer of the eye. This layer is of utmost importance as it provides almost the entire eye with blood. The cilliary body and its portion known as the pars plana are located behind the iris of the eye. It is in charge of production of aqueous humor, a specific fluid that nourishes the lens and the cornea and circulates through the front chamber of the eye.
Inflammation of the pars plana is typically accompanied by accumulation of white blood cells and the products they made by degradation at the very site of inflammation. They all fill the middle chamber of the eye and are the reason why patients report to see 'dots', 'streaks' or 'stuff' in their filed of vision. So white blood cells along with their by-products are to blame for visual problems patients suffering from pars planitis commonly have to deal with. What is more, during an eye exam a well experienced ophthalmologic also detect these floaters which fill the middle chamber of the eye.
The condition occurs alone or there are some other eye problems. For instance, one may also develop cataract or cystoids macular edema. In rare instances there are retinal vasculitis and neovascularisation i.e. formation of new blood vessels which makes matters worse and additionally jeopardizes the vision.
When it comes to underlying causes of pars planitis, the condition may be idiopathic (associated with no known cause) or develops together with some systemic diseases or as a complication of a systemic disease. Many scientists believe that inflammation of this portion of the uvea develops as a result of an immune mediated process.
Blindness of the Eye
The condition per se is not benign. It is estimated that around 20% of all patients suffering from pars planitis who are left untreated end up with substantial vision loss, some of them even lose their vision for good. Because of that doctors recommend thorough examination and aggressive treatment every time they suspect one is suffering from pars planitis.
Initially, patients are treated conservatively with medications while later some of them additionally require surgery that will improve the vision and remove all the particles associated with inflammation that have not been absorbed. Surgery is also efficient against progression of the disease.
Ocular immunologists or uveitis specialists are included in the treatment. It is essential to initiate the treatment as soon as possible because once the inflammation begins it simple cannot be reversed and may only progress causing more and more damage to the eye.
Systemic immunosuppression is the cornerstone of treatment. Local and topical therapy with eye drops is practically inefficient because drugs administered in such way cannot reach the affected parts of the eye and reduce inflammation. Better distribution of medications is achieved with injections. Corticosteroids, Prednisone in particular, are injected into the tissue around the eye. From there the drug is easily absorbed. Most doctors inject 6 doses being careful about potential complications such as an increase in intraocular pressure and resulting glaucoma. The treatment lasts approximately three to four weeks. In individuals in whom the inflammation is relatively difficult to treat doctors may implant a device in the eye which slowly releases corticosteroids within the period of two and a half years.
What is more, sometimes pars planitis may be associated with some infections, either bacterial or viral. In such case patients are additionally prescribed antibiotics or antiviral medications depending on the infectious agents. These medications are administered together with corticosteroids.
If corticosteroids fail to bring inflammation under control, patients are recommended other treatment options. The first one is immunosupression and the second is surgery. Aggressive immunosupression is achieved with cytotoxic agents. Also, there are several surgical procedures that may be performed. These include pars plana vitrectomy, endolaser therapy and cryotherapy.
Unfortunately, the inflammation may easily reoccur. Even after the most successful treatment patients may experience symptoms once against or their vision may get severely impaired. Still, with the available treatment most patients overcome the inflammation within the period of a few days to a few weeks.
And finally, even if the condition is diagnosed and treatment initiated on time, some patients suffer permanent vision loss. This is why any changes in the field of vision or any eye problems must be reported immediately to an eye specialist who will after performing an eye exam and certain tests diagnose the disease and recommend the best possible treatment preventing complications from occurring.
















Your thoughts on this
Loading...