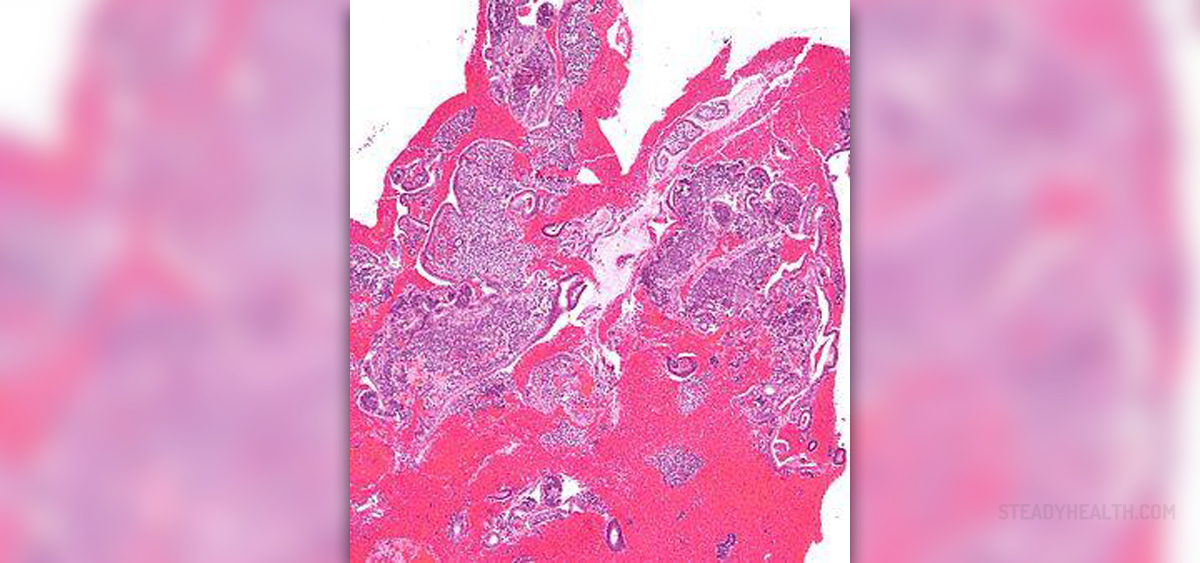
Endometrial resection, also known as hystero-resection is a procedure performed in women who are having menstrual problems. This is only one treatment option for this purpose and basically replaces hysterectomy (complete surgical removal of the uterus).
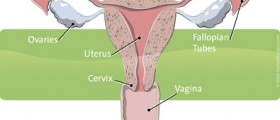
The procedure is always performed under general anesthesia because it may be very uncomfortable. In order to inspect the inside of the uterus doctors first insert a hysteroscope, assess the changes in the inner lining of the uterus, and then continue with the most convenient technique.
It is essential to memorize that endometrial resection is an invasive procedure capable to destroy much of the lining of the uterus. As a result, the woman is not supposed to get pregnant anymore. Pregnancy after endometrial resection is risky and may be associated with numerous complications. This is why she and her partner must choose the most efficient means of contraception and prevent undesirable pregnancy.
Endometrial Resection Techniques
Today, there are a few modern techniques doctors use while performing endometrial ablation. The most common ones are Thermachoice and Microwave endometrial ablation.
Thermachoice Uterine Balloon Therapy includes the insertion of a balloon into the uterus and its inflation. This way the balloon actually expands and gets into contact with the entire uterus. This is achieved with a sterile fluid. The fluid is at some point heated to 87 degrees and left inside the uterus for approximately 8 minutes. After the treatment, fluid is eliminated from the balloon, and the balloon is also removed from the organ.
Microwave Endometrial Ablation (MEA) is another widely used technique. It requires microwave energy in order to induce rapid, shallow heating of the endometrium. The heat is what destroys the endometrium. The entire procedure lasts no longer than 3 minutes.
- Randomised controlled trials (RCTs) comparing different endometrial ablation or resection techniques for women reporting HMB without known uterine pathology, other than fibroids outside the uterine cavity and smaller than 3 centimetres, were eligible. Outcomes included improvement in HMB and in quality of life, patient satisfaction, operative outcomes, complications, and the need for further surgery, including hysterectomy.
- We included in this update 28 studies (4287 women) with sample sizes ranging from 20 to 372. Most studies had low risk of bias for randomisation, attrition, and selective reporting. Less than half of these studies had adequate allocation concealment, and most were unblinded. Using GRADE, we determined that the quality of evidence ranged from moderate to very low. We downgraded evidence for risk of bias, imprecision, and inconsistency.
- Overall comparison of second?generation versus first?generation (i.e. gold standard hysteroscopic ablative) techniques revealed no evidence of differences in amenorrhoea at 1 year and 2 to 5 years' follow?up (risk ratio (RR) 0.99, 95% confidence interval (CI) 0.78 to 1.27; 12 studies; 2145 women; I² = 77%; and RR 1.16, 95% CI 0.78 to 1.72; 672 women; 4 studies; I² = 80%; very low?quality evidence) and showed subjective improvement at 1 year follow?up based on a Pictorial Blood Assessment Chart (PBAC) (
- Study results showed no difference in patient satisfaction between second? and first?generation techniques at 1 year follow?up (RR 1.01, 95% CI 0.98 to 1.04; 11 studies; 1750 women; I² = 36%; low?quality evidence) nor at 2 to 5 years' follow?up (RR 1.02, 95% CI 0.93 to 1.13; 672 women; 4 studies; I² = 81%).
- Compared with first?generation techniques, second?generation endometrial ablation techniques were associated with shorter operating times (mean difference (MD) ?13.52 minutes, 95% CI ?16.90 to ?10.13; 9 studies; 1822 women; low?quality evidence) and more often were performed under local rather than general anaesthesia (RR 2.8, 95% CI 1.8 to 4.4; 6 studies; 1434 women; low?quality evidence).
- Trials reported little or no difference between second? and first?generation techniques in requirement for additional surgery (ablation or hysterectomy) at 1 year follow?up (RR 0.72, 95% CI 0.41 to 1.26; 6 studies: 935 women; low?quality evidence). At 5 years, results showed probably little or no difference between groups in the requirement for hysterectomy (RR 0.85, 95% CI 0.59 to 1.22; 4 studies; 758 women; moderate?quality evidence).
Only women who are confirmed not to suffer from uterine fibroids or any other structural deformities of the inside of the uterus are suitable candidates for endometrial resection.
Before and After the Procedure
Prior to the procedure women are prescribed certain medications which reduce the thickness of the inner lining of the uterus. After being admitted into the hospital, the woman must sign a consent form and she is told everything about the procedure, including potential complications. It is essential to report all the allergies to medications or other allergens, previous surgeries, active diseases, and medications that are currently taken.
After the procedure many women are kept hospitalized overnight to recover. Cramping in the lower abdomen is a common side effect of the procedure and is brought under control with painkillers. Resting is essential for complete recovery. A woman must stay in bed for at least 24 hours after getting home.
An increase in body temperature or worsening pelvic pain are symptoms that must be immediately reported to the doctor because they point to some complications.














Your thoughts on this
Loading...