Sarcoidosis is a medical condition characterized by inflammation associated with the formation of specific nodules in multiple organs.
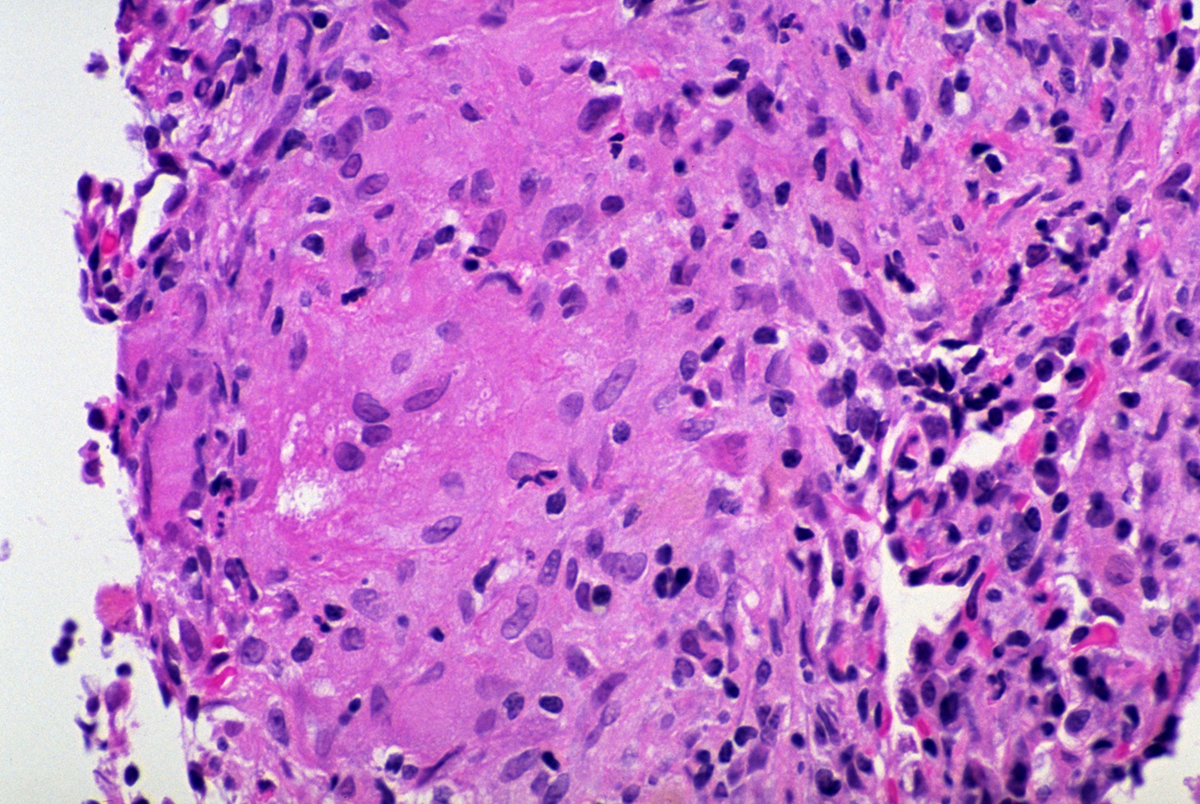
These nodules comprise inflammatory cells and are known under the name granulomas. In the majority of patients, granulomas form inside the lungs or lymph nodes although other organs and organ systems may be affected as well.
Classification of Sarcoidosis
There are various types of sarcoidosis. Annular sarcoidosis is the type affecting the skin. There are papular skin lesions organized in a typical annular pattern.
Erythrodermic sarcoidosis and ulcerative sarcoidosis are also cutaneous forms of the disease. They are rather rare. One more type of sarcoidosis affecting the skin is ichthyosiform sarcoidosis. The skin changes in this form of the disease look like the ones that develop in ichthyosis vulgaris.
Hypopigmentated sarcoidosis leads to hypopigmentation of the affected skin. It is typical for dark-skinned individuals.
Furthermore, mucosal sarcoidosis leads to the formation of pinhead-sized papules. Papules are also present in the case of papular sarcoidosis while scar sarcoidosis, as the name suggests leads to skin scarring. Subcutaneous form affects subcutaneous tissue and leads to the formation of deep-seated nodules.
Löfgren syndrome is a relatively rare form of sarcoidosis affecting only specific ethnic groups such as Scandinavian people. Lupus pernio is characterized by indurated skin lesions predominantly affecting the ears, nose, lips, or cheeks. This form resembles lupus vulgaris but is pathophysiologically different.
Morpheaform sarcoidosis is relatively rare causing severe fibrosis and cutaneous skin lesions. Neurofibromatosis affects the central nervous system. This form is commonly associated with sarcoidosis of other organs and rarely occurs alone.
And finally, there is systemic sarcoidosis, a condition characterized by collections of granulomas that affect practically almost every organ in the body.
Sarcoidosis - Symptoms and Signs
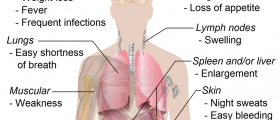
Patients suffering from sarcoidosis typically complain about fatigue, lack of energy, weight loss, aches, and pains. Cutaneous forms of the disease may be in many forms ranging from skin rash to scarring caused by severe fibrosis.
The heart is affected in approximately 20-30% of all patients but only 5% of these actually experience heart issues. In others heart involvement is asymptomatic.
If granulomas develop in the eye, the patient develops uveitis, uveoparotitis, and inflammation of the retina. These conditions are associated with loss of visual acuity and rarely complete loss of vision.
Neurosarcoidosis is characterized by granulomas forming on the basal meninges. The granulomas affect cranial nerves as well and depending on the affected nerve patients develop characteristic neurological symptoms and signs.
And finally, if the scalp is affected, a person may experience patchy hair loss.
Treatment and Prognosis
Most patients suffering from sarcoidosis require no treatment. As a matter of fact, treatment is considered not necessary in between 30 and 70% of all patients. Others, however, require medications that act against the formation of new granulomas and are additionally prescribed drugs that deal with current symptoms (symptomatic treatment).
Corticosteroids efficiently slow and sometimes even reverse the course of the disease. It is, however, possible that patients do not respond to corticosteroids. All in all, these medications are only indicated in case of severe and progressive sarcoidosis, affecting multiple organs, and interfering with their function.
Patients may be additionally prescribed azathioprine and methotrexate (both steroid-sparing agents) or cyclophosphamide, a chemotherapeutic agent.
It is possible for one to enter remission spontaneously. The disease may also progress and become chronic. Progression is rarely a cause of pulmonary fibrosis and associated lethal outcomes. The prognosis is not so positive if granulomas affect the heart.
Unfortunately, people with sarcoidosis are prone to certain cancers such as lung cancer or lymphomas. Leukemia (hairy cell leukemia, acute myeloid leukemia, and acute myeloblastic leukemia) may occur as well. This is the reason why apart from the primary disease, doctors should pay close attention and search for any sign of cancer in its early stage.
Relevant Data
The onset of sarcoidosis is gradual and the condition sometimes withdraws spontaneously. For instance, two-thirds of all patients suffer no symptoms 9 years after the beginning of the disease, Furthermore, half of all patients do experience relapse while only 10% of them end up with a severe disability.
- The incidence is 11 cases per 100,000 in whites but 34 cases per 100,000 in African Americans with a lifetime risk of 2.4 percent in the United States. Extrapulmonary sarcoid is seen in up to 25 to 30 percent of patients.
- Cardiac involvement is seen more commonly in males, while skin and eye features are more prominent in women. Extrapulmonary features can be different in terms of age of presentation, gender, and ethnicity.
- A key role in the development of sarcoidosis is played by T cells as they promote cellular immune reaction and are usually associated with an inverted CD4/CD8 ratio. It is well characterized by noncaseating granuloma typically containing macrophages, multinucleated giant cells, and epithelioid cells, in addition to lymphocytes, monocytes, mast cells, and fibroblasts There is a role of tumor necrosis factor (TNF) and TNF receptors, as both are increased in this disease. This has been evidenced by the role of anti-TNF agents, such as pentoxifylline and infliximab.
- Ocular manifestations are seen in close to 50% of patients, of which the most common clinical feature is uveitis. The CD4/CD8 ratio of vitreous lymphocytes has prognostic value. Heart block and sudden death have also been reported in sarcoidosis. Prophylactic insertion of an implantable cardioverter-defibrillator (ICD) is recommended in patients who develop cardiac sarcoidosis.
- The quality of life of symptomatic patients is poor. Many develop psychiatric symptoms, including depression and anxiety.
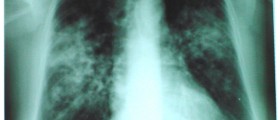
- For patients with pulmonary sarcoidosis causing worsening symptoms, stage II to III radiographic findings should be considered for oral glucocorticoids at 0.3 to 0.6 mg/kg for 4 to 6 weeks. If there is no improvement in symptoms, radiographic abnormalities, and pulmonary function tests, steroids may be continued for an additional four to six weeks. Maintainance steroids are not needed; steroid tapering to a dose of 0.25 to 0.5mg/kg (usually 10 to 20 mg) per day should be considered over a period of at least six to eight months.
- Data regarding mortality are not available because, in many cases, long-term follow-up is missing. Overall, it appears that about one-fifth of patients develop functional impairment, and there is a mortality rate of 3 to 5% in patients who are not treated. The highest mortality rates are in African American females past the fifth decade of life.














Your thoughts on this
Loading...