Degenerative bone disease is a term that can be applied to several conditions featured by degeneration of the bones.
Types of Degenerative Bone Disease: Osteoporosis
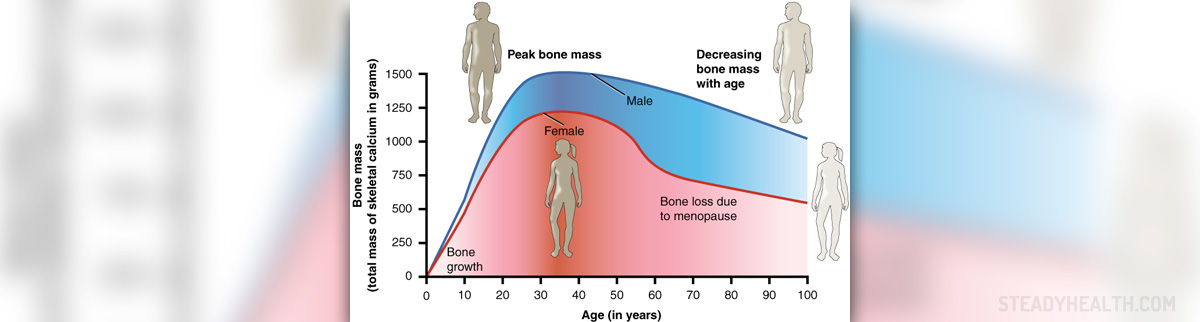
Osteoporosis is a disease in which bones become weak and brittle due to loss of bone density. Osteoporosis often results in bone fractures. Hips, spine, and wrists are particularly susceptible to fractures. Our bones are living tissues that are constantly changing. A new bone is created, and the old one is broken down. This process of remodeling helps our bones to heal, but at the same time, lifestyle and diet may affect it. After the age of 30, bone remodeling starts to slow down, and we lose more bone mass than we gain.
Women are particularly at risk of osteoporosis due to hormonal changes. In women, bone loss rapidly increases after menopause because of a decrease in levels of estrogen, a hormone that normally protects against bone loss.
- The 2010 Global Burden of Disease Study estimated that 10%–15% of all adults aged over 60 had some degree of symptomatic OA, with prevalence higher among females than males.
- Rheumatology traditionally defines OA as a condition marked by significant cartilage loss and joint space narrowing and OA classification criteria require the presence of radiographic bony changes or osteophyte formation in accordance with Kellgren and Lawrence standard.
- Early OA features proinflammatory factors that lead to the activation of proteolytic enzymes responsible for the degradation of the extracellular matrix (ECM) resulting in joint tissue damage. Although destruction and loss of the cartilage is a central component of OA, all joint tissues are progressively affected indicating that OA is a disease of the joint as an “organ”.
- Early OA is supported by pro-inflammatory mediators such as cytokines and chemokines that are in turn the consequence of the innate immune response to joint injury. In advanced stages of OA, additional inflammatory and pro-fibrotic modulators such as connective tissue growth factor (CTGF) together with transforming growth factor-beta (TGF-?) induce synovial and IFP fibrosis, further inducing articular cartilage destruction.
- In recent years several regenerative medicine procedures have been introduced for OA treatment. These treatments have the common aim of improving symptoms through tissue regeneration and restoring homeostasis to local cells. Unlike bone, articular cartilage is rather recalcitrant to regenerate.
- In 2001 the FDA issued a set of regulations governing cellular and tissue-based therapies. The basic principle of these guidelines was that cellular and tissue therapies that require minimal to no manipulation of autologous tissue do not required FDA approval, whereas those that involve any significant modification or treatment, including genetic manipulation, require approval.
- Joint replacement cannot often be offered to frail, elderly patients (ASA III-IV) due to high risks of complications and increase mortality. Likewise, surgeons are reluctant to offer younger patients joint replacement due to the limited life span of a prosthesis and chronic postural imbalance induced by the new joint. The result is the increasing consumption of chronic medications such as NSAIDs and opioids in so-called pain management. This palliation has a severe systemic backlash on patient care and health systems due to the complications related to chronic NSAIDs and opioids intake and addiction.
Paget’s Disease
Paget’s disease, also known as osteitis deformans, is a chronic condition that causes abnormal bone growth. In Paget’s disease, the bone remodeling process is disturbed, which results in bone that is brittle, enlarged, and susceptible to fracture.
Paget’s disease typically affects the spine, pelvis, skull, thigh bone, collar bone, and upper arm bone. This disease mainly affects adults, and it is estimated that between 2 to 3% of Americans suffer from Paget’s disease.
The exact cause of Paget’s disease is unknown. However, family history, as well as viral infection, represent the risk factor. Paget’s disease is usually asymptomatic and often incidentally discovered during X-ray tests performed for other reasons. Over time, Paget’s disease starts to manifest in bone pain and bone deformity. Depending on the affected bone different complications may result from the disease. For example, deformity of the skull can cause headaches and hearing loss.
Degenerative Arthritis
Degenerative arthritis, also known as osteoarthritis or degenerative joint disease, occurs due to inflammation, breakdown, and loss of the cartilage of joints. Degenerative arthritis commonly affects the hands, feet, spine, hips, and knees.
The disease is associated with symptoms such as joint pain, tenderness, stiffness, swelling, and limited movement of joints. Scientists have not identified what causes degenerative arthritis, but certain factors are known to increase the risk for the disease. The risk factors include family history, fractures, age over 45 years, and being a female.
Also, several medical conditions may contribute to the development of osteoarthritis. They are rheumatoid arthritis, Paget’s disease, gout, parathyroid disease, chronic kidney disease, and senile osteoporosis.
- medlineplus.gov/osteoarthritis.html
- www.cdc.gov/arthritis/basics/osteoarthritis.htm
- Photo courtesy of Partynia by Wikimedia Commons: commons.wikimedia.org/wiki/File:615_Age_and_Bone_Mass_DE.jpg
















Your thoughts on this
Loading...