Tylenol - Introduction
This is a North American brand of drugs advertised for relieving pain, reducing fever, and relieving the symptoms of cough, allergies, or cold. The active component of its original, flagship product, acetaminophen (known as paracetamol outside North America) is promoted as a painkiller.
Prevention of Complications Related to Tylenol
It should never be mixed with other medication, while that may be severely hazardous. Alcoholics should never take this medicine. Also, one should always consult a doctor and answer all the questions he might have, to better determine the dosage and use.

Symptoms
After ingesting large doses of this drug, one might not be experiencing any symptoms for up to a day. The symptoms of a Tylenol overdose are nausea (accompanied by vomiting), lack of appetite, abdominal pain, and feeling ill. Other symptoms may include sweating, an upset stomach, or convulsions.
Complications
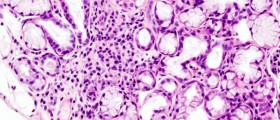
Being that, it is primarily metabolized in the liver, acetaminophen may overwhelm the way the liver functions. This is because it can cause elevations of liver enzymes in the blood suggesting injury to the liver. However, this is extremely rare.
It can harm the liver of those people who are alcoholics or have already had liver damage in the past. That is why, before using this medicine, one must consult a doctor and present him with any previous liver problems.
- Three physician toxicologists independently classified every in-hospital death associated with APAP overdose from eight large Canadian cities over three decades using the Relative Contribution to Fatality scale from the American Association of Poison Control Centres. The sensitivity and latency were calculated for each of the following criteria: King's College Hospital (KCH), Model for End Stage Liver Disease (MELD) ?33, lactate ?3.5 mmol/L, phosphate ?1.2 mmol/L 48+ hours post-ingestion, as well as combinations thereof.
- A total of 162 in-hospital deaths were classified with respect to APAP as follows: 26 Undoubtedly, 40 Probably, 27 Contributory, 14 Probably not, 25 Clearly not, and 30 Unknown.
- Cases from the first three classes (combined into n = 93 “APAP deaths”) typically presented with supratherapeutic APAP concentrations, hepatotoxicity, acidaemia, coagulopathy and/or encephalopathy, and began antidotal treatment a median of 12 hours (IQR 3.4–30 h) from the end of ingestion.
- Among all patients deemed “APAP deaths”, meeting either KCH or lactate criteria demonstrated the highest sensitivity (94%; 95% CI 86–98%), and the shortest latency from hospital arrival to criterion fulfilment (median 4.2 h; IQR 1.0–16 h). In comparison, the MELD criterion demonstrated a substantially lower sensitivity (55%; 43–66%) and longer latency (52 h; 4.4–? h, where “?” denotes death prior to criterion becoming positive).
- Identification of patients who are unlikely to survive without a liver transplant after acetaminophen poisoning is challenging.
- Several prognostic criteria exist, all of which have limitations, primarily the relatively long time duration from ingestion until criteria are met.
- The latency (i.e., time interval from hospital presentation until a given criterion is fulfilled) has not been well characterized nor compared between criteria.
- We discourage the use of the MELD score to prognosticate patients who present with acetaminophen-associated liver failure.
Over many years, it has been used countless times by many people, and it has proven to be a safe and effective medication for treating pains and relieving fever symptoms, although it has been shown to promote blood flow in some instances, which could be bad for people using blood thinners. However, if taken in excess amounts (overdose, whether on purpose or by accident), acetaminophen can cause life-threatening illness, and, sometimes, can lead to a coma.
The antidote to Tylenol overdose is N-acetylcysteine. It is most efficient when given within 8 hours of ingestion. It can prevent liver failure if given early on. That is why it is particularly essential that acetaminophen poisoning be recognized and treated as early as possible.
Although it has been proven safe, risks should not be overlooked. One might have liver problems. However, this happens only when an unusual amount of Tylenol has been ingested by the person. In that case, the person must go to the doctor immediately after this has happened to prevent other problems that may occur due to the Tylenol overdose.









,-Or-Ibuprofen-Which-Over-The-Counter-Painkiller-Should-You-Choose_f_280x120.jpg)





Your thoughts on this
Loading...