Introduction
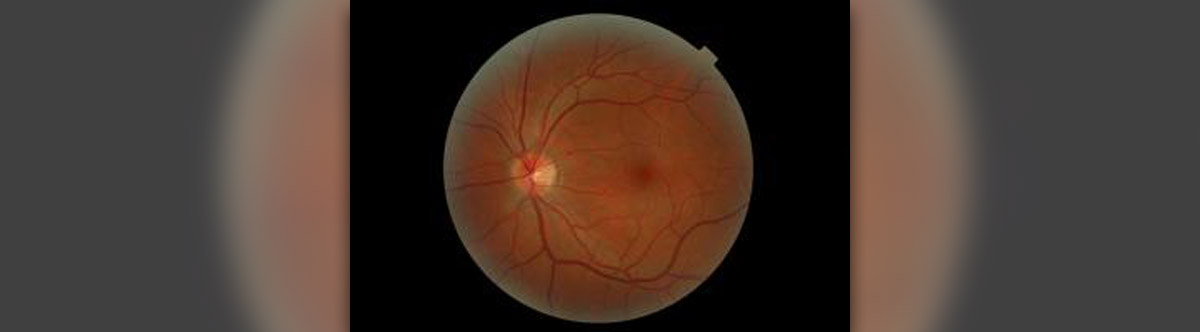
Retina is a part of the eye. This rather complex tissue actually covers the inner surface of the back of the eye. The role of the retina is to receive the light images. The process of focusing of these images is helped by two other eye organs called the cornea and the lens. After the light has reached the retina, a specific biochemical change occurs and the electrical impulses that are formed are further distributed via optic nerve into the part of the brain that is in charge with vision. The brain finally defines what we really see.
Retina is formed by two types of cells, the rods and the cones. The rods are in charge of night vision while the role of the cones is to sharpen the eye sight. In the very center of retina there is a macula. Peripheral part of retina which includes everything apart from macula is rather important as it helps us to notice and see the objects that are around us. This way retina helps us to move without bumping into people and surrounding things. On the other hand macula is important as it is in charge with more specific vision that is essential for reading and so on. This organ is as any other organ in the body well supplied with blood due to retinal arteries and veins.
Retinal Detachment
Retinal detachment is a condition in which retina disconnects from the layer it is lying on. The majority of detachments happen due to the breaks or tears of the retina. The vitreous gel is what keeps retina lying on the tissues below it. Now, if vitreous gel loosens the retina can detach. The problem starts when a part of retina has already detached and the tear is big enough to allow the entrance of vitreous gel. This way the gel may enter the tear and lead to further retinal detachment. In case that this condition continues the whole surface of retina can end up detached. In certain cases the tear is followed by the bleeding from retina blood vessels.
- In the current study, the majority of patients were repaired with scleral buckle alone (71%), and final anatomic reattachment rate was 95%. The predominance of scleral buckle alone as the primary treatment choice in this study is consistent with treatment modalities reported in patients with RRD in this age group.
- In a recent retrospective review of RRD repair in 512 patients, primary scleral buckle was the most common means of repair in patients aged 21–40 years (15/23 (65%) scleral buckle, 8/23 (35%) primary pars plana vitrectomy alone), with primary pars plana vitrectomy alone more common in patients aged 40 years or older. In a recent review of RRD repair in 3403 eyes in the United Kingdom National Health Services, a considerably lower average age was reported in patients who were repaired with SB alone (39.2 years) compared to pars plana vitrectomy (62.6 years) or combined scleral buckle/pars plana vitrectomy (58.4).
- The use of scleral buckle for primary repair in younger patients may reflect the lack of posterior vitreous detachment and the phakic lens status, with an effort to preserve accommodation given the higher incidence of cataract development in phakic eyes that undergo initial pars plana vitrectomy. Pars plana vitrectomy alone was not considered due to the age of the patients and the lack of posterior vitreous detachment in this age group. The incidence of interim cataract extraction between time of primary repair and last clinical visit was significantly higher in the scleral buckle/pars plana vitrectomy group (7/11 (64%)) compared to the scleral buckle group (3/27 (11%)).
- Retinal dialysis was noted in 6/38 (16%) eyes despite no reported history of trauma. This may suggest a remote history of or unrecognized trauma in these patients. However, idiopathic, nontraumatic retinal dialysis has been reported to occur in young adult eyes, potentially attributable to a developmental abnormality of the retinal periphery or vitreous base.
- In the current study, overall anatomic success was 95%, consistent with overall reattachment rates in recent literature. Prior retinal detachment in the fellow eye was present in 13% of cases, slightly higher than observed rates of 2–10% in the adult population and likely reflective of the presence of high myopia in the current study.
Possible Complications of Retinal Detachment Surgery
The goal of the surgery is to find all the breaks on the retina and to fix them. There are several procedures that can be performed in this case.
Some patients face no complications at all. Others may complain about slight discomfort and watering of the operated eye. The eye may be red and with edemas. Itchiness can be present for certain period of time. Luckily, all the previous problems can be easily solved with eye drops.
In small number of patients blurred vision can persist for several months. This condition requires new spectacles with changed diopter.
In case of scleral buckle surgery one may suffer from double vision. Glaucoma, which is the condition that features with increased pressure within the eye, is another possible complication.
Bleeding can affect different parts of the eye. The blood can collect into the vitreous, in the retina or behind it. The worst complications include cataract and dropping of the eyelid. They require additional surgical procedure. And finally, if the patient is not administered proper antibiotics even infection can occur.
















Your thoughts on this
Loading...