Melanonychia is a condition in which an individual's nail/nails are affected by brown or black pigmentation. In longitudinal melanonychia there are pigmented stripes along the length of the nail bed. Longitudinal melanonychia is also known as melanonychia striata. The condition can be associated with some not so serious medical diseases such as systemic disorders, trauma, inflammatory disorders, fungal infections or intake of certain medications. However, it is also connected with more severe ones such as subungual melanoma. Benign melanocytic hyperplasia is another potential cause of longitudinal melanonychia.
Melanonychia Pathophisiology
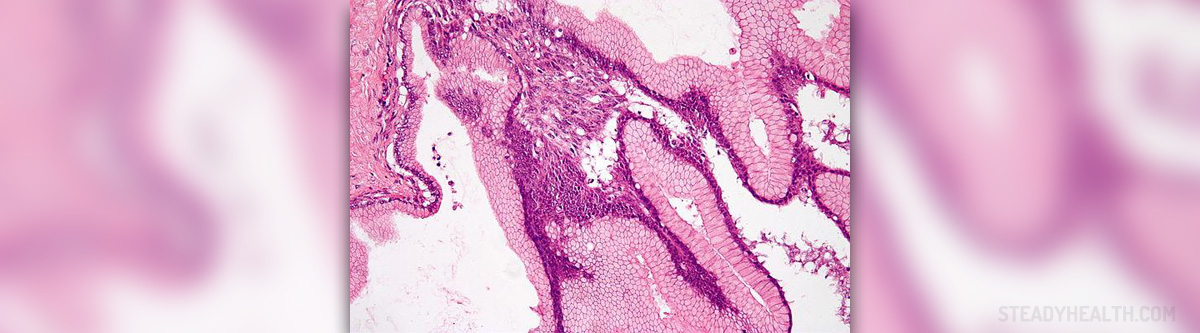
The specific pigmentation of the nail unit develops as a consequence of increased production of melanin, a pigment synthesized in melanocytes (cells located in the skin and mucous membranes). Normally, there are around 200 melanocytes per 2 mm in the nail matrix and most of them are dormant. Still, once these cells become more active melanosomes containing melanin get transferred into differentiating matrix cells. They eventually migrate to distal parts of the nail and transform into nail plate onychocytes. The final effect of such transformation is increased pigmentation of the nail plate.
Melanonychia Treatment
Patients who have developed melanonychia and are currently suffering from certain systemic disorders and illnesses must have their condition brought under control and the problem with nails will resolve. Furthermore, melanonychia associated with intake of certain drugs can also be easily dealt with once the person stops taking the drug that has led to nail pigmentation.
It is best to perform a biopsy of the suspicious tissue and pathohistological examination of the taken samples. Patients who refuse biopsy must undergo a dermatoscope examination and are due to be monitored. Biopsy is particularly indicated in case a doctor suspects on melanoma.
Melanoma is a highly lethal type of skin cancer. Individuals whose melanonychia is connected to this cancer require more complex treatment approach and total excision of the nail apparatus (Mohs micrographic surgery). Invasive melanomas are treated with amputation of the distal phalanx of the affected finger. Patients with more invasive melanoma also require sentinel lymph node biopsy which confirms or rules out spread of the tumor cells into regional lymph nodes. Further treatment after tumor excision depends on the stage of the disease and requires consultation and treatment monitoring by a well experienced oncologist.
Certain number of patients may develop postoperative nail dystrophy. This complication is more frequent after biopsy of the proximal part of the nail.The prognosis of melanonychia associated with systemic diseases and medications is excellent while people who have developed melanoma do not have chance to complete cure unless the cancer is treated in the early stage of the disease. This is why any kind of nail pigmentation (particularly brown and black ones) should be reported as soon as possible.









_f_280x120.jpg)







Your thoughts on this
Loading...