Motor neuron disease (MND) is also known as Lou Gehrig’s disease or amyotrophic lateral sclerosis or ALS. You may also hear some doctors referring to it as Charcot's disease, syndrome or even Charcot's sclerosis. In general, MND is found in some 5 to 7 of 100.000 people and doctors in general practice witness one or two cases during their career. According to some statistics, men over 80 years of age are more likely to develop this condition than elderly women of the same age.
About Motor Neuron Disease or Lou Gehrig’s Disease
This disease is very rare, but people suffering from it are faced with progressive paralysis and potential death. MND affect motor neurons, causing dysfunction of lower motor neuron (LMN) and upper motor neuron (UMN) and provoking muscular paralysis. Patients usually have mixed LMN/UMN paralysis, although LMN symptoms are usually more dominant.
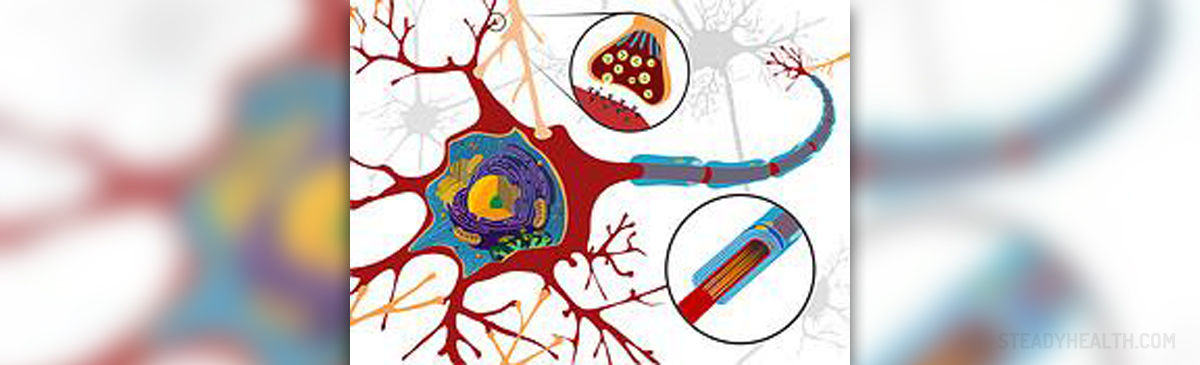
No one knows why some people get this disease. However, current medical theory believes that abnormality of mitochondrial function can be responsible for oxidative stress in motor neurons and therefore damage of LMN and UMN.
Motor Neuron Disease Symptoms
MND symptoms usually include focal onset of ALS, which affects both upper and lower motor neurons. It could have three different patterns, affecting the limbs (limb onset, which is the most common start of this disease) and bulbar onset, which is present in some 20% of all ALS patients. Additionally, patients may also have respiratory onset of this disease, but happens very rarely.
MND may also be presented only with UMN or only with LMN features. Pure upper motor neuron features of the disease are known as primary lateral sclerosis, while patients diagnosed with pure LMN features are known to have progressive muscular atrophy.
Possible Health Complications and End Stage Care
There are numerous complications of MND and patients may suffer from many health-related problems. Constipation, spasticity and cramps of the muscles and urinary tract infections are probably the least serious. However, these patients may also suffer from pneumonia, depression, immobility and attendant disability, some complications because of immobility, such as: bedsores, skin infections or ulcer, as well as some cognitive deterioration and finally respiratory failure and death.
Care in patients diagnosed to be in end stages of this disease usually requires hospice care and symptom management. Opiates may be useful for respiratory distress, lorazepam for choking episodes, while subcutaneous morphine may resolve present dyspnea. Also, some advanced directives may be given from the patient, in order to implement his or her wishes regarding the treatment.
Palliative Care in MND
The progression of the disease is very individual, but there is usually progressive loss of muscle power, which may affect the limbs, the bulbar area – affecting speech and swallowing – and the respiratory muscles of the chest wall and the diaphragm. The usual cause of death is respiratory failure, often associated with infection. There are now two drugs licensed for MND – riluzole, which has been shown to slow the progression in some patients, and edaravone, which has been shown to help certain patient groups and is licensed in the United States.
- Palliative care has a very important role in the care of patients with motor neuron disease and their families. There is increasing emphasis on the multidisciplinary assessment and support of patients within guidelines, supported by research. This includes the telling of the diagnosis, the assessment and management of symptoms, consideration of interventions, such as gastrostomy and ventilatory support, and care at the end of life. The aim of palliative care is to enable patients, and their families, to maintain as good a quality of life as possible and helping to ensure a peaceful death.
- Many guidelines stress the need for palliative care including the European Federation of Neurological Societies, the US Practice Parameter and the National Institute of Health and Care Excellence (NICE) Guideline NG42 Motor neurone disease: assessment and management. There is also increasing discussion of the need for close collaboration between neurology and palliative care services, with increasing education of all involved.
- There is increasing evidence for the effectiveness of palliative care in MND. A study, in a mixed group of 50 patients with neurological disease, including 16 people with MND, in Turin, Italy, showed that the involvement of the palliative care team improved quality of life and there was clinical improvement in symptoms – pain, dyspnoea, sleep disturbance and bowel symptoms. Moreover, there was no increased mortality in the intervention group, compared with a control group, showing that palliative care was safe as well as effective.
- There is increasing evidence of the presence of cognitive change in MND and that nerve loss is not only found in motor neurones but within the brain, and in particular the frontal lobes. Up to 50% of patients with MND may have cognitive impairment and this may be seen as:
(1) Fronto-temporal dementia (FTD) – for up to 15% of patients, and especially those with the C9orf72 gene mutation (which is also associated with FTD alone).
(2) ALS bi – behavioural impairment, seen in up to 28% of patients with evidence of frontal lobe dysfunction.
(3) ALS ci – cognitive impairment occurs in up to 39% of patients and may be seen with behavioural changes. These changes may be found on testing, but there is increasing evidence that they are also clinically relevant.
- Depression is seen more commonly in MND, particularly in patients over 65 years and in the first year after diagnosis. Rates in studies vary from 4.4% to 12%. The use of antidepressants was also higher in MND, although tricyclic antidepressants may also be given to help with drooling. Although the wish to die was common, with 25% of patients expressing these wishes, the majority did not have depression, with only 37% of this group showing evidence of clinical depression.
- There is increasing evidence that death for MND is usually peaceful and studies have shown that choking of death is rare – in a study of patients at St Christopher’s Hospice in London only one patient died choking, and this was in 1968 soon after the hospice opened; in a further study of 121 patients in the United Kingdom and Germany, no patient died choking and over 88% patients died peacefully.
- Some patients with MND may wish to discuss hastening of death – by euthanasia or physician-assisted suicide. In countries where this is legal, there is evidence that people with ALS do chose an assisted death more often than other people – in Oregon the rate of physician-assisted suicide was 374.5/10,000 compared to 61.0/10,000 for cancer and in the Netherlands about 20% of patients with ALS receive euthanasia compared to 5% of cancer patients or 0.5% of heart failure.















Your thoughts on this
Loading...