Introduction
When blood that is supposed to return from the lower extremities to a heart returns very slowly, a condition named chronic venous insufficiency occurs, or short CVI. There are numerous reasons why this condition appears, and they can be labeled as age, venous thrombosis, unhealthy lifestyle, congestive heart failure, diabetes mellitus and bad habits such as smoking.
Symptoms of Venous Insufficiency
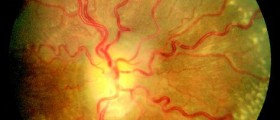
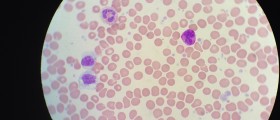
How can one know that he has chronic venous insufficiency? Symptoms that indicate this condition are, in most cases, a swollen leg or arm, varicose veins, itching, etc. Ulcers that can’t heal can also indicate the presence of this disease. The color of the skin in the place where it occurs is usually red because of the presence of a large number of red blood cells. If a person experiences these symptoms, he should visit a doctor who can diagnose chronic venous insufficiency. It is conducted with radiological tests, venograms, and duplex ultrasounds.

Treatments
The process of chronic venous insufficiency treatment is done in two steps. The first step is the treatment of CVI complications with decongestive therapy for the edema or swelling. Then, in the second part of the treatment, the main attention is on the actual cause of the CVI. The treatment itself consists of two parts, surgical and non-surgical. Non-surgical therapy presents the process of treatment with massages, a compression pump, Unna boots, chronic ulcerations, and sclerotherapy.
Not everyone will undergo the surgical part of the treatment; it only applies to patients who have CVI due to congenital anomalies of poor or nonexistent vein valves. There are also treatments that are done in order to stop other accompanying symptoms (itching, infections, and ulcers) that can be very unpleasant.
Complications
There are a number of complications that can appear due to chronic venous insufficiency. At first, pain and paresthesia appear and are followed by many complications. It is of big importance to get help if you suspect CVI, because if you don’t, a number of other severe complications may develop. Some of them are the recruitment of the veins, infections, injuries to veins and arteries, skin burns, venous thrombosis that can be very deep, and many other complications.
- For many patients, the progressive loss of the cosmetic appearance of their legs is the prime cause for seeking treatment. Unsightliness is not confined to tortuous dilated veins but includes telangiectasias (“spiders”) and reticular veins.
- Symptoms of venous insufficiency are highly variable. Patients report a spectrum of discomfort ranging from fullness or heaviness, dragging or aching, to frank pain. Occasionally, throbbing and itching may occur. The pain is exacerbated by standing, is progressive throughout the day, is typically felt in the muscles in the calf or thigh, and is relieved by rest and limb elevation. It is also frequently relieved by the wearing correctly fitted gradient support hose.
- Ankle edema associated with uncomplicated varicose veins is usually mild and becomes more noticeable as the day progresses. Edema associated with deep system insufficiency is more severe and may be persistent.
- Thrombophlebitis is a common complication of varicose veins, perhaps because their prominence makes them more susceptible to local trauma. It is thought that this seldom occurs spontaneously and an episode of minor trauma or a period of bed rest is often associated.
- Bleeding from large varicosities typically follows local trauma; however, bleeding may occasionally occur spontaneously. Elderly patients with thin-walled veins are at increased risk. Patients may be unaware of the venous rupture and first notice the problem when they feel blood running down the leg or even after feeling faint.
- Although most patients are acutely aware of skin changes associated with venous disease, occasionally, patients with varicose veins may fail to notice minor skin changes in the lower leg because they are so slow to develop. On the other hand, some patients may be anxious and seek evaluation because of the fear of deterioration in their condition. O'Leary et al found that this was a reason for referral in 14% of patients.
- Prolonged venous hypertension resulting in venous dilatation and passage of red blood cells through the endothelium into the interstitium results in breakdown and conversion of hemoglobin to hemosiderin. This remains as a brown pigment stain on the skin.
- With time, chronic inflammatory changes resulting in fibrin and hemosiderin deposition with local edema can result in venous dermatitis or varicose eczema. This can be either dry and scaly or vesicular and weeping. With progressive loss of epithelium, venous ulceration may develop spontaneously. In most cases, however, ulcers begin as the result of minor local trauma. Contact dermatitis can be seen in response to medications or even the rubbing of elastic bandages.
- Progressive fibrosis of the skin and subcutaneous tissues induced by chronic venous hypertension is referred to as lipodermatosclerosis but is sometimes called fat necrosis, folliculitis, or chronic cellulitis. It may occur acutely or in a chronic condition. The acute form eventually progresses to become chronic, but the chronic variety can develop spontaneously.
- Skin necrosis with replacement by scar tissue but without ulceration or sloughing results in small areas or patches on skin that are usually gray-white in color and usually only a few millimeters in size. These lesions, known as atrophie blanche, are associated with depression on the skin surface, are colored with thin transparent epithelium, and are sometimes surrounded by a halo of fine dilated venules.
- In addition to causing great individual distress, ulcers have serious economic and psychological effects and are a considerable drain on medical resources. It is estimated that between 300,000 and 400,000 patients suffer from venous ulcers in North America.
If a person who has CVI doesn’t treat it, the disease can progress, and as time passes by, ulcers that can’t heal will develop, and tissue will begin to atrophy and stain leading to insufficiency syndrome, thromboembolism, and internal bleeding. Sadly, the result of all of that is death.














Your thoughts on this
Loading...