Bleeding from the rectal area is a common sign of many gastrointestinal diseases, especially if it's in a terminal part of the rectum. Bleeding from this area can be in the form of blood, which is mixed with stool, in the form of traces of blood in the stool, or the bleeding may occur even if one does not pass any stool. No matter which of these presentations occurs, the condition is considered pathological and requires prompt diagnosis and appropriate treatment.
Causes of Bleeding from Rectal Area
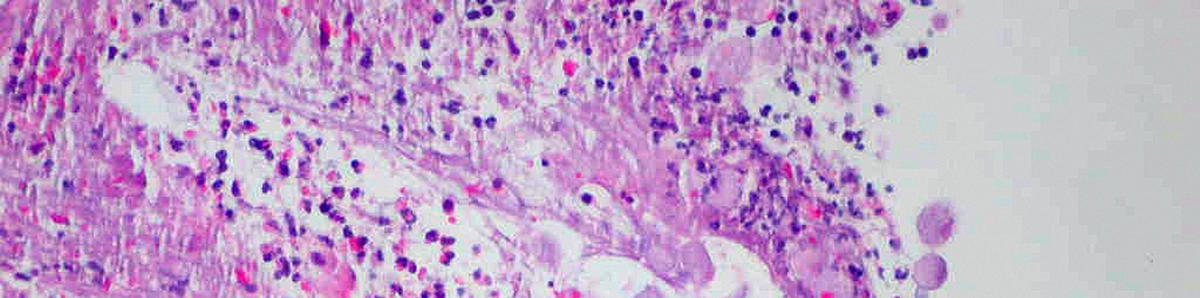
This is a common sign of several inflammatory illnesses of the large intestine. It affects people suffering from inflammatory bowel disease, ulcerative colitis, and Crohn's disease. Inflammatory bowel disease affects either the small or large intestine and may feature traces of blood in the stool.
Ulcerative colitis can affect the rectum, and the bleeding is, in this case, in the form of fresh blood and, in severe cases, it may be profuse. And finally, in Crohn's disease, a patient may notice bright red blood in the toilet bowl or darker blood mixed with the stool.
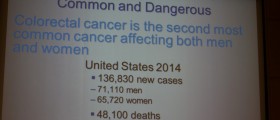
Another common cause of bleeding from the rectal area is colorectal cancer. In case the cancer affects proximal portions of the large intestine the blood is generally mixed with stool, while rectal cancer features bright red blood, which may be noticed on toilet paper.
- The Association of Coloproctology of Great Britain and Ireland, along with the Royal College of Surgeons, have recently updated their guidance on commissioning for the elective management and onward referral for diagnosis, investigation, and management of patients who experience rectal bleeding. It is not intended to guide commissioning relating to suspected cancer, and pathways already exist for: patients >50 years with unexplained rectal bleeding, who qualify for 2-week referral as per National Institute for Health and Care Excellence guidance; asymptomatic patients in the NHS Bowel Cancer Screening Programme; investigation of occult gastrointestinal bleeding; or emergency management of major lower gastrointestinal haemorrhage.
- The 2-week referral pathway tends to be a colorectal cancer exclusion service, so does not always benefit the symptomatic patient with rectal bleeding. There may be little attention paid to the presenting symptoms once cancer has been excluded.
- Best practice in primary care will include careful attention to history: presence or absence of perianal symptoms, red-flag symptoms including weight loss, altered bowel habit, symptoms of anaemia, and family history of colorectal cancer. Rectal bleeding alone has a positive predictive value for colorectal malignancy of only 8% in patients aged >50 years presenting to primary care.
- Nearly one-third of rectal cancer patients are younger than 55 years of age and if a rectal cancer does bleed it will likely produce bright red blood and not necessarily mixed with stool. Rectal bleeding attributed to haemorrhoids represents the most common missed opportunity to establish a cancer diagnosis.
- Endoscopic assessment of the bowel is the gold-standard investigation for bleeding, but other tests may be useful in selected cases. Complete endoscopic evaluation of the colon is indicated in select patients but didactic age cut-offs for colonoscopy and flexible sigmoidoscopy are difficult. Older patients will need to have a full colon investigation as appropriate, whereas younger, low-risk patients with rectal bleeding should be considered for flexible sigmoidoscopy. If other symptoms are present or there is a family history, then colonoscopy may be indicated.
- Anal fissures with an atypical appearance or clinical signs of chronicity with scarring or tags should be referred to secondary care. Topical treatments are unlikely to be effective in the face of scarring, and alternative diagnoses may need to be considered.
Constipation can lead to serious problems with defecation. The hardened stool may be difficult to pass, and it can damage the lining of the rectum and cause rectal bleeding. Even anal fissures, which represent cracks in the tissue of the anal canal, can cause occasional bleeding.
And finally, there are two more causes of bleeding from the rectal area, rectal prolapse and hemorrhoids. In rectal prolapse, parts of the rectum protrude through the anus. The friction of the external part may cause irritation and damage to the superficial layer and result in bleeding. Hemorrhoids are nothing but inflamed rectal veins which may bleed usually during defecation.
Evaluating Bleeding from Rectal Area
The best method to evaluate and identify the cause of rectal bleeding is to perform a colonoscopy. The procedure includes the insertion of a flexible tube into the anus. The tube is slowly moved to the upper parts of the large intestine, and with the assistance of a tiny little camera, a doctor can visualize the inner surface of the colon and find structural abnormalities or inflammation responsible for the bleeding. Once the underlying condition is identified the doctors recommend the most suitable treatment modality.
Bleeding from the rectum and anal area must never be neglected, and if it occurs, it must be reported as soon as possible. This way, even the diagnosis of serious conditions (such as malignant tumors), may be set on time and treated successfully.















Your thoughts on this
Loading...