Disturbance of heart’s rhythm which arises in the atria of the heart is known as atrial tachycardia. This problem may affect people with completely normal hearts, but also those whose hearts have some structural abnormality (caused by congenital diseases or some heart surgery).
Atrial tachycardia (AT) by definition belongs to the group of supraventricular tachycardias (shortened as SVT). This type of arrhythmia doesn’t require AV (atrioventricular) junction, ventricular tissue or some accessory pathways to be initiated or maintained. On the ECG (electrocardiogram), atrial tachycardia looks like narrow QRS complex tachycardia. Patients heart rate can be anywhere from 100 up to 250 bpm (beats per minute), while the atrial rhythm remains regular. Conducted ventricular rhythm could be producing conduction patterns such as 2:1, 4:1 or some combination of these patterns.
Classification of Atrial Tachycardia
Doctors may use different methods to classify atrial tachycardia. Anatomy, endocardial activation mapping data and pathophysiologic mechanism are the most commonly used criteria.
Anatomically, atrial tachycardias are differentiated on the location of the arrhythmogenic focus.
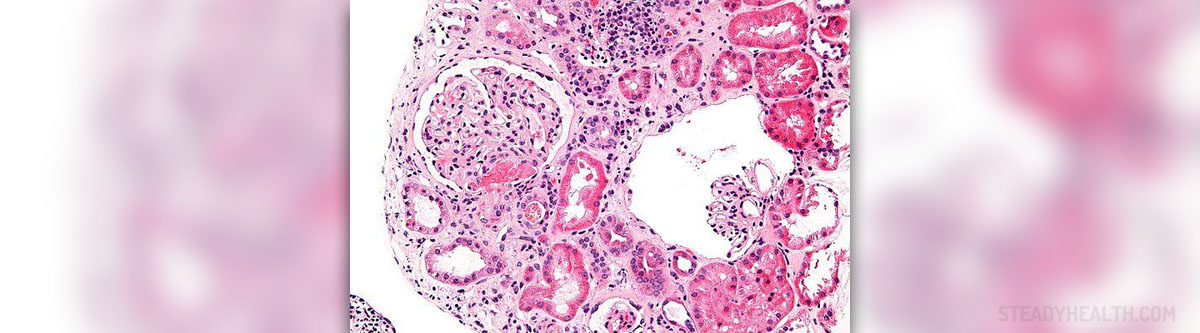
According to the endocardial activation, atrial tachycardia can be either focal or reentrant. Focal AT occurs in localized areas of the atria. It can arise in the pulmonary veins, ostium of the coronary sinus, intra-atrial septum or in crista terminalis. Reentrant atrial tachycardia is commonly macroreentrant and it mainly affects people with complex or structural heart diseases or patients after heart surgeries (during which the atria was incised or scarred).
Pathophysiologic mechanism differentiates enhances automaticity AT, atrial tachycardia with triggered activity and reentry AT.
Acute Atrial Tachycardia Causes
Patients with no structural anomalies of the heart can suffer from atrial tachycardia. People with congenital heart disease may also develop AT post operatively, after procedures to correct the problem. In these people, AT may pose a life threat.
Intoxication of digitalis, structural disease of the heart, ablation of the left atrium and gaps in ablation lines may all lead to development of acute tachycardia.
Condition known as multifocal AT or MAT is frequently associated with some other medical problem, such as myocardial infarction, valvular heart disease, methylxanthine toxicity, diabetes mellitus, lack of kalium (potassium) or magnesium, azotemia, pneumonia or sepsis.Diagnosis and Treatment
In order to identify, locate and differentiate atrial tachycardias, doctors commonly use the 12-lead ECG. Some cases may require certain laboratory or some electrophysiologic studies to exclude different systemic disorders as causes of AT.
Acute atrial tachycardia must be taken under control and doctors use AV blocking agents for that purpose. Calcium channel blockers or beta blockers are frequently used in these cases.
Cardioversion and radiofrequency catheter ablation are other possible options for the treatment of AT. Cardioversion is recommended for patients where drugs have proven to be inefficient or can’t be used for some reason, but also for people who don’t tolerate the rhythm well hemodynamically. Patients with symptoms of atrial tachycardia who don’t want long term drug treatment or who have been found out as medically refractory are treated with radiofrequency catheter ablation.
















Your thoughts on this
Loading...