Lower intestinal infection occurs due to any pathogen that affects the gastrointestinal tract in the body. Pathogens are tiny organisms that include virus, bacteria or parasite. Depending on the cause the infection in the intestines can vary from mild to severe. Some intestinal infections can result in lethal outcome if not adequately treated on time.
Causes for Lower Intestinal Infection
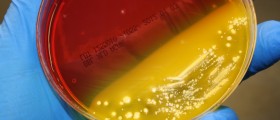
Intestinal infections are commonly caused by large number of microorganisms. Following bacteria are the usual cause of intestinal infections in people: Escherichia coli, Shigella spp, Staphylococcus, Salmonella spp, Vibrio spp, Campylobacter spp, Clostridium spp, Bacillus spp and Listeria spp. Viruses that usually lead to lower intestinal infection include: Rotaviruses, Hepatitis A virus, Adenovirus, Toroviruses, Coronavirus, Picornavirus and Herpes virus. A parasitic infection within the intestines includes worms such as: Flatworms, Roundworms, Tapeworms, and Hookworms.
People are commonly infected with these bacteria and viruses through ingestion of contaminated food and water. This is most commonly undercooked meat, unpasteurized milk and dairy products, and foods that are allowed to sit at room temperature for longer period of time. People can also be infected by swimming or drinking contaminated water. Disease that most frequently leads to lower intestinal infection is gastroenteritis or stomach flu that usually results from viruses such as adenovirus and parovirus or bacteria like Staphylococcus aureus and Escherichia coli. Lower intestinal infection can also result from diseases like gastritis, food poisoning, food borne disease and typhoid fever. Each of these conditions occurs because of contaminated food or water intake.
- 95 SARS-CoV-2-infected patients were involved into study with special emphasis on GI symptoms. Overall, 58/95 cases (61.1%) showed evidence of GI symptoms with diarrhoea (24.2%), nausea (17.9%), vomiting (4.2%) and impaired liver function as assessed by elevated transaminases (32.6%) being the most relevant features.
- Another study investigated 73 SARS-CoV-2-infected hospitalised patients in China and 53.4% patients were tested positive for virus in the stool ranging from day 1 to 12 of infection. Importantly, in this study, >20% of infected patients had positive virus in faeces even after clearance of virus in the respiratory tract. Similar results from Singapore showed that 50% of their COVID-19 patients had detectable faecal virus but only approximately half of these patients suffered from symptoms such as diarrhoea.
- Therefore, evidence is accumulating that GI symptoms are common and SARS-CoV-2 can be detected in faeces in about 50% of infected subjects but there appears to be no clear correlation of GI symptoms and detectable virus in the stool.
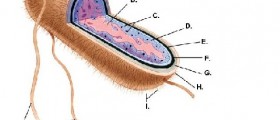
- A prerequisite of CoV infection is its entry into the host cells. Akin to its relative SARS-CoV, SARS-CoV-2 uses Angiotensin converting enzyme-2 (ACE2) as a viral receptor to enter host cells, and ACE2 is an important regulator of intestinal inflammation. By analyzing single-cell RNA sequencing data, researchers found that ACE2 was highly expressed in the small intestine especially in proximal and distal enterocytes. They also found that two other viral entry receptors for human coronavirus 229E virus and Middle East respiratory syndrome CoV virus were highly expressed in enterocytes.
- In about 50% of COVID-19 cases, the presence of SARS-CoV-2 in faecal samples and detection of SARS-CoV-2 in intestinal mucosa of infected patients suggest that enteric symptoms could be caused by invasion of ACE2 expressing enterocytes and the GI tract may be an alternative route of infection. In over half of the patients, faecal samples remained positive for SARS-CoV2 RNA for a mean of 11 days after clearance of respiratory tract samples.
Symptoms of Lower Intestinal Infection
Symptoms that are commonly associated with lower intestinal infection include nausea and vomiting. Abdominal cramps, pain, loss of appetite and diarrhea are also caused by intestinal infections. Fever, headache, jaundice and weakness are also the symptoms. Apart from that infected person commonly experiences sleep disorders, skin rash, dizziness and teeth grinding. Intestinal infections are typically followed by weight loss. In severe cases of intestinal infection muscle spasms, joint pain, swelling of some parts of the body and mental problems can be experienced by affected person.
Treatment for Lower Intestinal Infection
Diagnosis is made with the help of blood and urine tests. Initial treatment includes medications for diarrhea and vomiting. If intestinal infection is caused by bacteria the treatment involves antibiotics. There are also medications for viral and parasitic infection. Bed rest is generally recommended while hospitalization may be needed in severe cases. After recovering, it is advised to eat freshly cooked food and drink clean drinking water to prevent reoccurring of the intestinal infection.













Your thoughts on this
Loading...