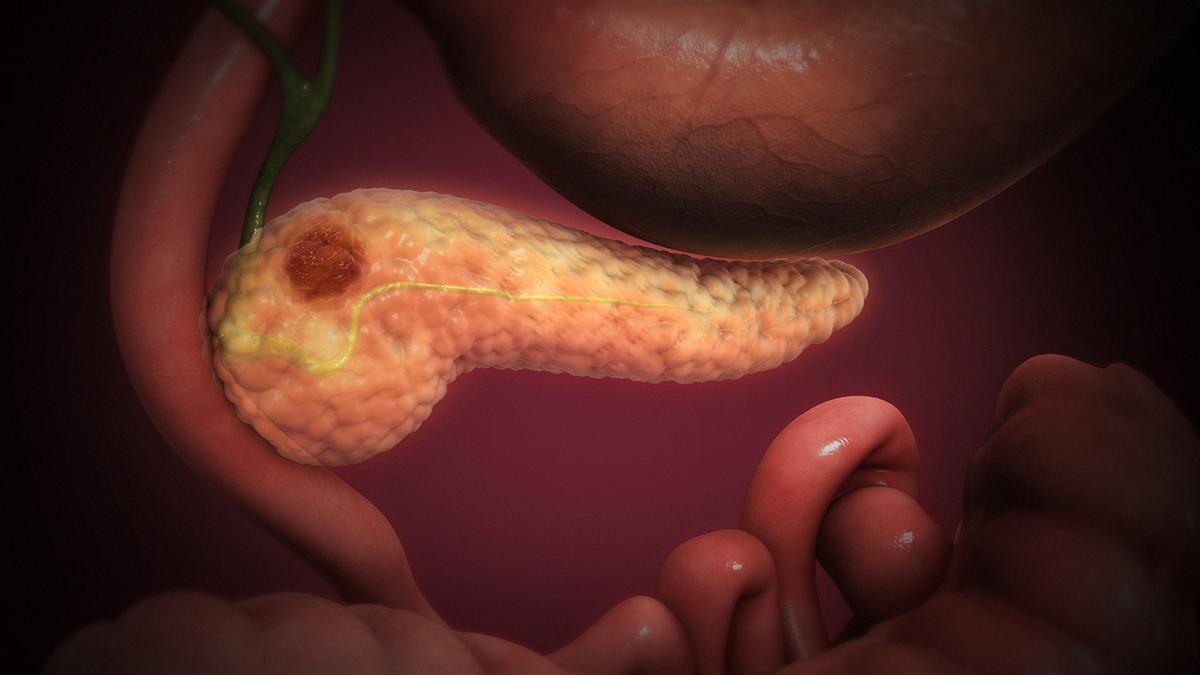
Pancreatic Cancer - Overview
Pancreatic cancer is one of the most malignant tumors in the body. The anatomy of this gland and its location allows the growth of the tumor and easily spread onto the surrounding organs. This is why many cases of pancreatic cancer are diagnosed in the third or fourth stage of the disease. The fourth stage (IV) is the terminal or end stage of pancreatic cancer. This stage features a variety of symptoms and signs, and it includes rapid deterioration of the patient and death.
Pancreatic cancer usually starts in the head and neck of the gland and it may originate from the exocrine or endocrine tissues. Still, the majority of pancreatic carcinomas are pathologically classified as adenocarcinomas.
This malignant disease predominantly affects men. It may occur due to genetic predisposition, poor diet, smoking, obesity, and diabetes. This malignant disease is also more frequent in patients older than 60 and those suffering from chronic pancreatitis.
Unfortunately, the number of patients diagnosed with pancreatic cancer has increased in the last few years. The major problem is that the diagnosis is usually set in an advanced stage of the disease when patients can only benefit from symptomatic and palliative treatment.
Symptoms of End Stage Pancreatic Cancer
In the end stage of pancreatic cancer, apart from infiltration of the regional lymph nodes, the tumor may affect all the nearby organs and tissues and can even give distant metastases. At the time of diagnosis, the regional spread of the tumor is identified in approximately 25% of all patients, and even up to 52% of patients have metastases in distant organs.
The symptoms and signs of stage IV pancreatic cancer depend on the affected organ. Still, the most common symptoms and signs of pancreatic cancer include jaundice (infiltration of the liver), severe skin itching, sharp abdominal pain, loss of appetite and weight loss, digestive problems, nausea and vomiting, dizziness, excessive bloating, and diarrhea.
The prognosis of end-stage pancreatic cancer is poor. The patients cannot be operated, and they usually do not respond to chemotherapy. Radiation therapy can only be applied in a limited form of the disease hence is useless in the end stage of this malignant disease.
Diagnosis of end-stage pancreatic carcinoma can easily be set after certain tests and examinations among which a CT scan or MRI of the abdomen give a perfect insight into the presence of the tumor and they also identify the spread of the disease to surrounding organs. Definitive diagnosis can be set after pathohistological examination of the biopted tissue.
- A retrospective cohort analysis of end-of-life (EOL) care outcomes of patients with pancreatic cancer who died between 2012 and 2016. Key indicators of aggressive cancer care in the last 30?days of life used were: ?1 emergency department (ED) presentations, acute inpatient/intensive care unit (ICU) admission, and chemotherapy use. We examined time from PCR to death and place of death. Early and late PCR were defined as >?90 and???90?days before death respectively.
- Out of the 278 eligible deaths, 187 (67.3%) were categorized as receiving a late PCR and 91 (32.7%) an early PCR. The median time between referral and death was 48?days. Compared to those receiving early PCR, those with late PCR had: 18.1% (95% CI 6.8–29.4%) more ED presentations; 12.5% (95% CI 1.7–24.8%) more acute hospital admissions; with no differences in ICU admissions.
- Pain and complications of cancer accounted for the majority of overall ED presentations. Of the 166 patients who received chemotherapy within 30?days of death, 23 (24.5%) had a late PCR and 12 (16.7%) an early PCR, with no association of PCR status either unadjusted or adjusted for age or gender. The majority of patients (55.8%) died at the inpatient palliative care unit.
- www.nhs.uk/conditions/pancreatic-cancer/treatment/
- www.cancer.gov/types/pancreatic/patient/pancreatic-treatment-pdq
- Photo courtesy of https://www.scientificanimations.com via Wikimedia Commons: commons.wikimedia.org/wiki/File:3D_Medical_Animation_Acute_Pancreatitis.jpg
















Your thoughts on this
Loading...