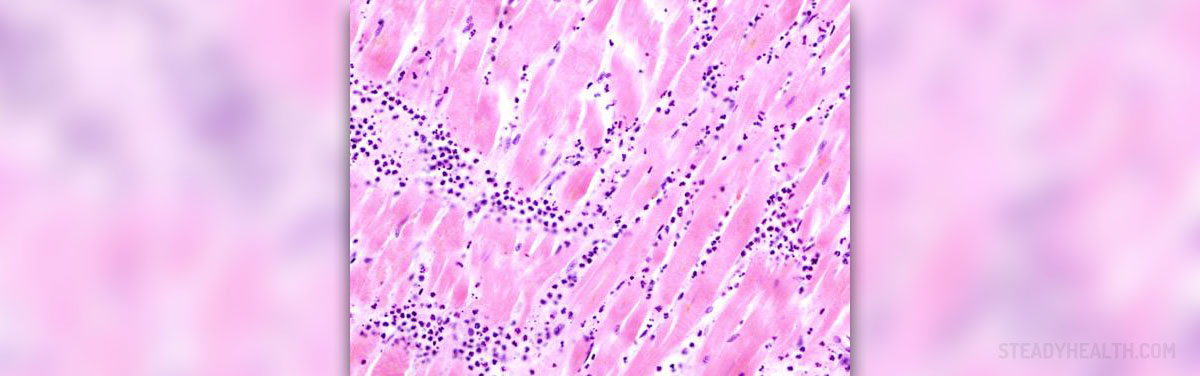
Multiple sclerosis, also known as MS, is an inflammation of the fatty myelin sheaths that are wrapped as a protective layer around axons of the brain and spinal cord. When the inflammation affects these sheaths, it gradually damages the layer, leading to demyelination and scarring.
When this happens, the conduction of signals in the affected nerves is impaired, and this results in various problems in sensation, movement, cognition, and other functions. The exact type of impairment depends on which nerves are involved in demyelination. This is a rare condition that affects between two and 150 individuals per 100,000.
Acute Multiple Sclerosis
Acute multiple sclerosis is also known as Marburg-type multiple sclerosis, malignant or fulminant multiple sclerosis. Some experts classify acute multiple sclerosis as a separate disease, while others consider it one of the multiple sclerosis borderline diseases.
This is the most severe type of multiple sclerosis that is usually lethal. However, there is some evidence that acute multiple sclerosis responds to Mitoxantrone, Alemtuzumab, and autologous stem cell transplantation.
Acute multiple sclerosis is very aggressive and advances quickly and uncompromisingly. It involves severe loss of myelin sheaths, leading to rapid disability and death. This form of multiple sclerosis usually affects young people and it is preceded by fever.
Causes of Multiple Sclerosis
There is no known definite cause for multiple sclerosis. Currently, scientists believe it is an autoimmune disorder where the damage is caused by the patient’s immune system when it starts to attack its own nervous system. It seems like this disease develops out of a combination of genetic, environmental, and infectious factors.
Even though it has a genetic component, multiple sclerosis is not a hereditary disease. This genetic predisposition possibly makes people more vulnerable to certain risk factors.
There are many environmental factors associated with this disease and living farther from the Equator seems to be the most important one. People living closer to the North or South Pole have less sun exposure and they are generally more prone to decreased vitamin D production.
Unmanaged stress may also be one of the factors, as in any other autoimmune disorder, but there is not enough evidence to support this claim. Exposure to toxins, smoking habits, hormonal intake, and dietary factors are also considered possible causes of multiple sclerosis.
Certain infections are also proposed as potential causes for multiple sclerosis. Infection with human herpes viruses or Epstein-Barr virus may also increase an individual’s risk of contracting multiple sclerosis.
- Multiple sclerosis affects about 85 000 people in the United Kingdom and is the most common cause of neurological disability in young adults. The National Institute of Clinical Excellence (NICE) has recently published management guidelines that highlight the need to improve standards of care offered to people with this condition.
- Multiple sclerosis typically presents between 20 and 40 years of age. Women are more susceptible than men by a factor that approaches 2:1. Race and geography also affect susceptibility to the disease. As a general rule, although with clear exceptions, the risk of multiple sclerosis increases with increased distance from the equator. Migration studies have also suggested that environmental factors in childhood may have an aetiological role.
- The proportion of people with benign disease is a minority and decreases with length of follow up. For example, in an Irish study 42% of people had benign disease after 10 years but this had decreased to 34% after 15 years.
- Diagnosis may be straightforward when a person presents having had two discrete neurological episodes suggestive of multiple sclerosis disseminated in space and time with objective evidence on examination. However, people may present in a number of ways that cause difficulty in diagnosis.
- An acute relapse refers to an episode of neurological disturbance, of the kind seen in multiple sclerosis, that lasts for at least 24 hours, and for which there is no other cause such as fever. Typically a relapse evolves over a few days, reaches a plateau, and then remits to a variable degree over a few weeks or months. The patient experiencing a relapse has to cope with a comparatively sudden onset of neurological symptoms that may be physically and psychologically distressing and functionally and socially incapacitating. In the longer term, incomplete remission from a relapse may result in residual neurological deficit.
- Management of an acute relapse requires a comprehensive approach addressing its medical, functional, and psychosocial effects. Management incorporates education regarding relapses, support in the event of a relapse, treatment to accelerate or improve the recovery from a relapse, and symptomatic treatment and rehabilitation. The other area of management is to reduce the frequency of relapses with disease modifying therapies such as interferon beta. Disease modifying therapies are not discussed here but have been reviewed extensively elsewhere.
- Several general health factors have been proposed to affect relapse activity in multiple sclerosis. Infections may trigger a relapse or exacerbate existing symptoms. Where possible infections should be anticipated and treated early. An association has been reported between common viral infections and relapse but these are difficult to avoid. Infections may occur as a complication of multiple sclerosis, for example urinary tract infections due to retention, and chest infections due to aspiration, so addressing their underlying causes may be preventative.







-and-Multiple-Sclerosis-Differences-And-Similarities_f_280x120.jpg)







Your thoughts on this
Loading...